INTRODUCTION
Post-infectious cerebellitis is an inflammatory condition of the cerebellum, often occurring after a viral or bacterial infection. It presents with ataxia, dysarthria, nystagmus, and other cerebellar dysfunctions. While the condition is usually self-limiting, early diagnosis and appropriate management are crucial for better patient outcomes. This article presents a case of post-infectious cerebellitis in a 42-year-old male, detailing his presentation, diagnostic approach, and treatment course.
CASE PRESENTATION
A 42-year-old gentleman was transferred to our emergency department (ER) from an outside hospital with complaints of slurred speech, loss of balance, and difficulty in standing and walking for the past two days. He was initially evaluated at another hospital, where an MRI brain on day 1 and an MRI brain with whole spine contrast on day 2 were reported as normal. Due to persistent symptoms, he was referred for further management.
HISTORY & CLINICAL EXAMINATION
The patient had a history of fever with cough and yellow-colored expectoration 10 days prior, which was treated at a local clinic with intravenous antibiotics for three days. The fever and respiratory symptoms had resolved three days before his current symptoms appeared.
On primary survey, the patient’s vital signs were stable, with a Glasgow Coma Scale (GCS) of 15/15, a heart rate of 104 bpm, respiratory rate of 26 bpm, blood pressure of 130/80 mmHg, and SpO₂ of 99%. There were no signs of airway obstruction or systemic instability.
A secondary survey revealed no known drug allergies (NKDA), no past medical or surgical history, and no recent intake of neurotoxic substances. His medications from the previous hospital stay included Inj piperacillin-tazobactam (4.5 g TDS), Inj doxycycline (100 mg BD), Tab aspirin (150 mg OD), and Tab atorvastatin (20 mg HS).
CNS EXAMINATION
Higher functions: Normal
Cranial nerves: No facial asymmetry, pupils equal and reactive (2 mm bilaterally)
Motor system: Power 5/5 in all four limbs, normal tone, and deep tendon reflexes (DTR) 2+ bilaterally
Horizontal nystagmus
Dysarthria+
Dysmetria with intention tremor (positive finger-nose test and heel-knee test)
Broad-based ataxic gait
Positive Romberg’s test (swaying to the left)
Bilateral plantar reflexes: Flexor response
INVESTIGATION
Laboratory Results
Arterial Blood Gas (ABG): Normal pH (7.44), normal PCO₂ (39), and bicarbonate (27.1)
Complete Blood Count (CBC): WBC count of 14,200/uL (mild leukocytosis)
Electrolytes: Sodium 133 mEq/L, potassium 4 mEq/L, chloride 103 mEq/L
Renal Function Tests (RFT) & Liver Function Tests (LFT): Within normal limits
ECG: Normal sinus rhythm, heart rate 91 bpm, no acute ST-T changes
Additional Tests Ordered:
Blood cultures (2 sets)
Serology tests (for viral and bacterial causes)
Vitamin B12 levels
Nerve conduction study
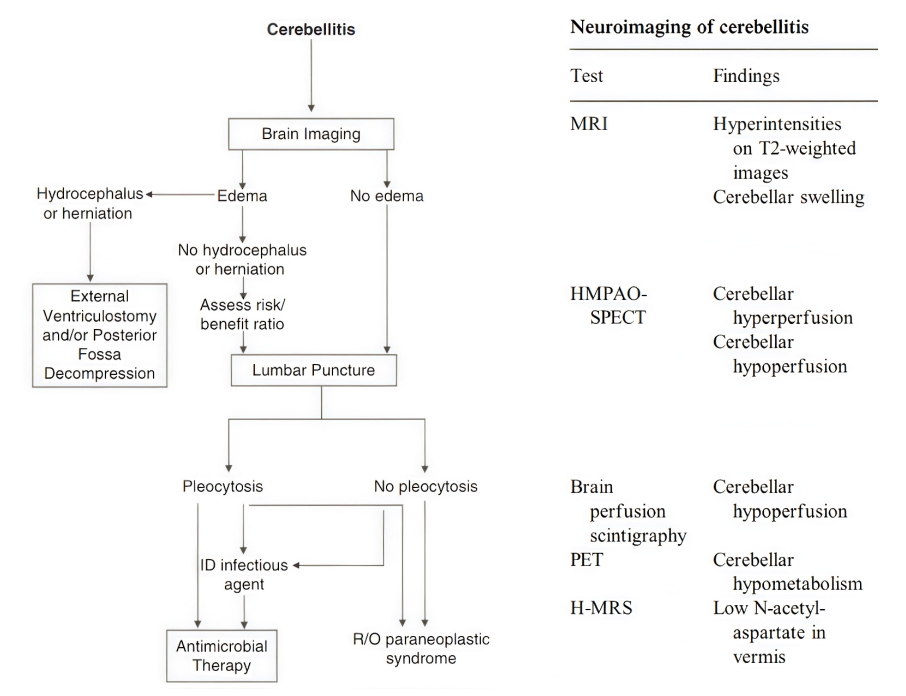
Based on clinical findings and the absence of structural abnormalities on MRI, a diagnosis of post-infectious cerebellitis was made.
Treatment and Outcome
Day 1 : The patient was started on intravenous methylprednisolone (1 g IV OD for 3 days).
Day 2 : Improvement in dysarthria was noted.
Patient was able to walk with one-person support.
Steroid therapy was continued.
Day 3 : Patient was shifted to the ward for continued monitoring.
Day 4 (Discharge Plan)
The patient showed significant improvement, being able to walk independently with subtle ataxia.
Discharged with a tapered dose of oral prednisolone (Wysolone) for 15 days.
Follow-up was advised to assess complete recovery and rehabilitation.
DISCUSSION
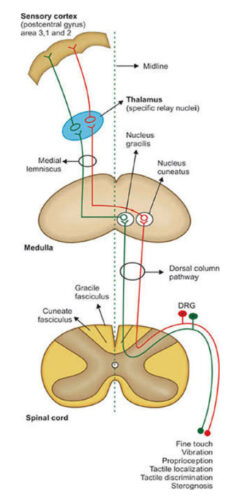
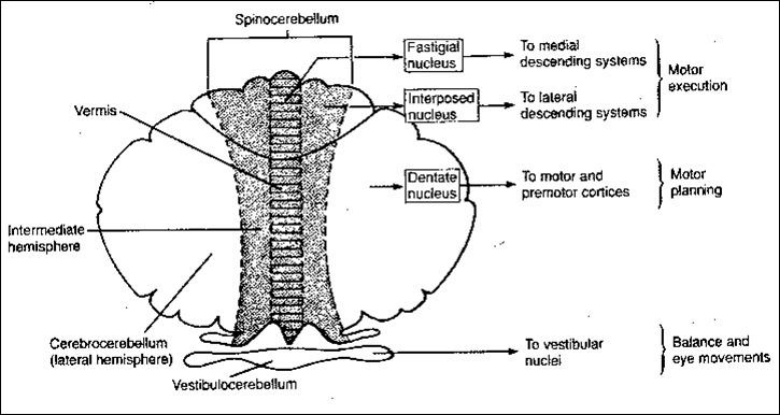
Ataxia is a neurological condition characterized by impaired coordination, which can result from dysfunction in the cerebellum and its connections, the proprioceptive sensory pathway, or the vestibular system. Understanding the underlying pathophysiology and differentiating between these types of ataxia is essential for accurate diagnosis and effective management.
APPROACH TOWARDS ATAXIA
Ataxia can be classified based on the affected system:
- Cerebellar Ataxia – Results from dysfunction of the cerebellum or its pathways. It typically presents with dysarthria, intention tremor, nystagmus, and gait disturbances.
- Sensory Ataxia – Caused by impaired proprioception due to damage to the dorsal column pathway (e.g., Vitamin B12 deficiency, Tabes dorsalis). Patients have a positive Romberg’s test but lack other cerebellar signs like nystagmus and dysmetria.
- Vestibular Ataxia – Arises from peripheral or central vestibular dysfunction. It presents with vertigo, nystagmus, abnormal head impulse test, and sometimes hearing disturbances (e.g., vestibular neuritis, aminoglycoside toxicity).
- Romberg’s Test and Sensory Ataxia
Romberg’s test assesses the patient’s ability to maintain balance with their eyes closed.
 Dr. Avinash. S
Dr. Avinash. S Dr. Ashok Nandagopal
Dr. Ashok Nandagopal