Rehabilitation in Parkinson’s Disease
Need for Rehab in Parkinson’s Disease:
Rehabilitation has an important role in providing independent living. In addition, known complications of PD can be reduced or prevented while the quality of life is promoted. Optimal management involves a coordinated interdisciplinary team to oversee a comprehensive plan of care to address the patient’s individual clinical problems, concerns and needs. The team typically includes the rehabilitation physician, nurse, physiotherapist, occupational therapist, speech-language pathologist and social worker. Referral to other specialists may also be necessary, which includes a psychologist, nutritionist, gastroenterologist, urologist, pulmonologist and so forth. As with any team, the patient is the central figure, with family and caregivers being key members. Rehabilitation should be offered to these patients right from the start to encourage an active lifestyle and to improve quality of life.

Goals of PD in Physiotherapy Aspect:
Physiotherapy has a significant importance in a multidisciplinary team focused on the rehabilitation of individuals with PD, with the purpose of maximizing functional ability and minimizing secondary complications through movement rehabilitation within a context of education and to support the person as a whole.
To maximize quality of life depending on stage of disease:
- Promote full functional ROM in all joints
- Correct faulty postures – prevent contractures and deformities
- Minimize disuse atrophy and muscle weakness
- Enhance postural awareness
- Promote functional gait
- Enhance balance reactions and safety measures
- Maintain or increase vital capacity, chest expansion
- Maintain functional independence
- To conserve energy of the patient and care takers
- Maintain or improve endurance
- Assist in psychological adjustment to chronic disability and life-style modifications
- Prevent falls and teach how to get up after a fall
- Suggest appropriate walking aids
Outcome Measures for PD:
- Timed Up and Go Test (TUG):
To determine fall risk and measure the progress of balance, sit to stand and walking. Cut off scores indicating risk of falls by population (in seconds); PD -11.5. - Six Minute Walk Test (6 MWT):
The 6 Minute Walk Test is a sub-maximal exercise test used to assess aerobic capacity and endurance. The distance covered over a time of 6 minutes is used as the outcome by which to compare changes in performance capacity.In neurology conditions, the 6 MWT has been implemented in the assessment of those patients and it has been regularly used to capture any changes. An increase in the distance walked indicates improvement in basic mobility.
- 10 Meter Walk Test:
The 10 Meter Walk Test is a performance measure used to assess walking speed in meters per second over a short distance. It can be employed to determine functional mobility, gait and vestibular function.Measure of function which correlates to balance and fall risk. ≤ 10 seconds – normal; ≤ 20 seconds – mobility without gait aid; ≤ 30 seconds – requires gait aid; ≥ 14 seconds – indicates high risk of falls.
- Berg Balance Test and Rating Scale:
The Berg Balance Scale (BBS) is used to objectively determine a patient’s ability (or inability) to safely balance during a series of predetermined tasks. Cut-off score of 56 indicates functional balance and score of ‹ 45 indicates individuals may be at greater risk of falling.
Occupational Therapy and Parkinson’s Disease
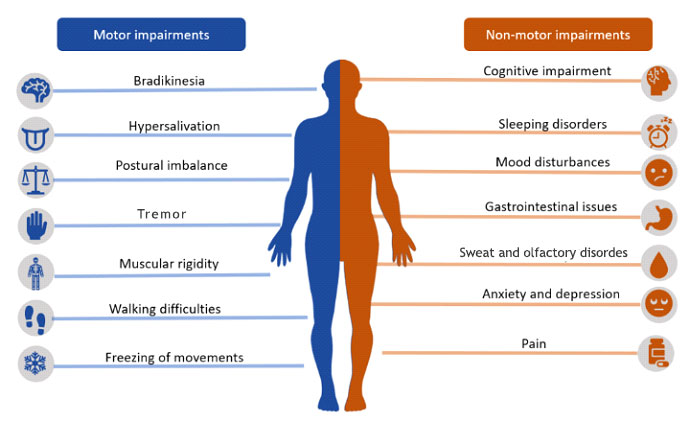
Parkinson’s disease is a progressive disabling neurodegenerative disease. Symptoms can include several problems with movement such as stiffness, slowness, tremors during movement or at rest, and sometimes non-motor symptoms such as issues in communication, mood, vision and problem-solving abilities. Occupational therapists support individuals with Parkinson’s disease by enabling them to maintain their usual level of self-care, work and leisure activities for as long as possible.
Strategies Employed:
- Employ patient’s personal strengths
- Modify or adapt the environment
- Adapt the activity
Areas Focused:
- Fall Prevention: Aimed at reducing the risk of falls, therapists recommend people with PD to pay full attention and concentrate on walking and use alternative and augmentative aids such as pockets, diagonal shoulder bags, body belts or trolleys.
- Sit-to-Stand Transfers: Sit-to-stand transfers from chairs, toilets and the bedside may present difficulties for people with PD. Occupational therapists provide appropriate strategies such as using suitable worded verbal cues and suggest equipment to aid transfers including chair risers, riser recliner armchairs and level-access showers instead of a bath.
- Bed Mobility: Skills such as turning, adjusting a position and getting out of bed are taught to the patient.
- Posture and Seating: Therapists help increase awareness and self-correction of postural problems, assess the need for postural support and review wheelchair suitability.
- Eating and Drinking: Eating and drinking modifications such as ideal sitting posture and adequate lighting are recommended to create a distraction-free environment.
- Self-Care Routines: This is focused on helping individuals with PD whose personal care routines have become slow and tiring, which in turn increases the risk of falls.
- Domestic Skills: Loss of coordination and balance in addition to a reduced multitasking ability can affect meal preparations, housework and shopping activities. Small items such as non-slip latex for easier jar opening, lever taps when using taps, and a wire mesh to help drain pans or vegetables may be introduced to help promote day-to-day activities thereby reducing effort. Adaptations for housework such as ironing, maintenance tasks and management of paperwork may be required.
- Fatigue Management: People with PD may become tired more quickly due to the effort of staying upright and inefficient movement strategies. Therapists help in scheduling the daily roles and routines, help prioritize tasks, restructure activities according to energy levels, and introduce regular resting periods, including good sleep.
- Handwriting: People with PD might have micrographia, or handwriting difficulties where letters are smaller and sloping toward page corners instead of straight across. Visual or auditory cues as well as sitting comfortably and in an upright position at a table with good lighting may help in the betterment of handwriting.
- Driver evaluation and vehicle modification information for appropriate usage and handling of private and public transport.
- Leisure skill development for enhancement of personal development and occupational life performance.
- Work simplification and energy conservation techniques for daily life activities.
Role of Speech Language Pathologists
People with Parkinson’s (PD) may notice changes or difficulties in communication and swallowing. These changes can happen at any time, but tend to increase as the disease progresses. Just as PD affects movement in other parts of the body, it also affects the muscles in the face, mouth and throat.
Speech and Swallowing Difficulties Seen in PD
- Softened voice, reduced volume in voice
- Speaking in an unchanging pitch (monotone)
- Having a hoarse or strained quality voice
- Having a breathy voice
- Tremor in voice
- Slurring of speech
- Short rushes of speech
- Loss of facial expression
- Difficulty in chewing and swallowing
Treatment
A speech-language pathologist (SLP) can help pick the right approaches for the existing communication and swallowing difficulties. In general, treatment for individuals with PD includes behavioral approaches or alternative and augmentative devices (AACs) for their communication and swallowing problems.
Specific treatments for volume and clarity of speech such as Lee Silverman Voice Treatment (LSVT) LOUD and Parkinson Voice Project SPEAK OUT!, are carried out by certified therapists.
Communication devices to enhance or amplify speech, also may be helpful. These include personal microphones, touchpads and gadgets that prompt you to speak up if your voice volume decreases.
For swallowing difficulties, exercises to strengthen swallowing muscles, as well as diet modifications such as thickening liquids are recommended. Several behavioral strategies such as not using drinking straws, tucking your chin to your chest when swallowing and taking smaller, slower bites when eating are also suggested.
Role of Clinical Psychologist
Parkinson’s disease is a disorder that leads to a lot of changes in the neurotransmitters in the brain, which can result in depression, anxiety and even hallucinations. It can also run in families as a result of genes being passed from one generation to next. The role of the family members in handling such patients becomes a stressful situation. On the other hand, people with PD have a lot of sleep issues, where the daytime sleeping pattern is high with 50% of patients affected.
The PD psychological symptoms are:
- Depression
- Anxiety
- Hallucination
- Delusion
- Psychosis
- Impulsive and compulsive behaviors
- Cognitive dysfunction
- Disorders of sleep and wakefulness
The following are the areas where the PD patient needs to be enhanced/nurtured based on the condition from mild to severe stage. Thus, the stage V is the final stage where the patient requires complete holistic care in life.
- Changes in Mood
- Changes in Thinking
- Executive functioning
- Attention
- Processing speed
- Memory
- Language
- Visual-spatial skills
There are many ways by which psychologists and neuropsychologists can help patients with Parkinson’s disease and their families.
- Adjustment issues need to be handled in a different manner based on the level of the condition.
- Anxiety and depression can be treated in addition with teaching skills to improve sleep quality.
- Need to evaluate changes in mood and cognition and make necessary recommendations towards maximum patient’s strength.
- Regular professional help needs to be taken at balanced intervals for the patients as well as family members.
Thus, 50% of the PD patients experience depression at some point of time in the course of the disease; major depression 5-20% and minor depression 10-30%, due to which it can worsen functioning and lead to poorer quality of life. Also, it increases the difficulty of the caregivers, when recognized or un-treated.
Psychological symptoms are common in PD and it is best thought of as a “neuropsychiatric” disorder. Bring psychological problems up with your doctor if you or someone close to you notices changes in your mood, thinking or behavior. There are a number of treatments that can be helpful for the psychological symptoms of PD.

Dr. G. Balamurali
Head of Spine Service, Consultant Spine and Neurosurgeon
Dr Lakshmi Nair, Consultant Physical Medicine and Rehabilitation
Mrs Janet M, Occupational Therapist
Ms Arul Jothi G, Physiotherapist
Ms Vedhavalli V, Physiotherapist
Ms Roshni Suresh, Clinical Psychologist
Ms Meghana S, Speech & Language Pathologist

