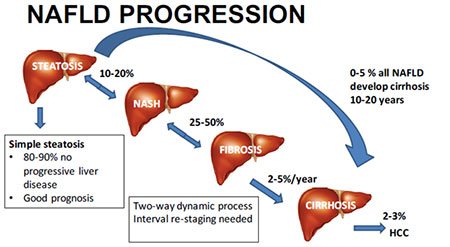
Non-alcoholic fatty liver disease (NAFLD) comprises non-alcoholic fatty liver (NAFL) and non-alcoholic steatohepatitis (NASH). NAFLD together with their complications of cirrhosis (shrinkage), liver failure and liver cancer will be the predominant liver disease for the conceivable future.
NAFLD has now replaced viral hepatitis as we have moved to complete cure for Hepatitis-C with oral antivirals medications for 3-months duration and lifelong oral antiviral therapy for hepatitis B infection and also cancer surveillance. NAFLD was observed to be 2 times more prevalent in men than women.
People with NAFLD are likely to be without any symptoms of the disease and incidentally diagnosed following abnormal liver function tests during routine blood tests or Ultrasound imaging. NAFLD can cause liver dysfunction related symptoms like fatigue, malaise and dull right-upper-abdominal discomfort. Mild jaundice may be noticed.
NAFLD patients should be investigated for metabolic risk factors (e.g., metabolic syndrome-obesity, diabetes mellitus (insulin resistance), dyslipidemia (high cholesterol levels), persistently elevated liver enzyme levels, increasing age and BMI (body mass index), endocrine gland disorders and hypoxia (low blood oxygen levels) caused by obstructive sleep apnea (airway disorder).
Causes of fatty liver unrelated to NAFLD are excessive alcohol use (over 30g for men and 20g for women), drug-induced steatosis (fat deposition), hepatitis C and endocrine conditions.
Also Read:What is Fatty Liver Disease?
Non-obese people affected by NAFLD (“lean NAFLD”) – have impaired insulin sensitivity, to be frequently sedentary (life style), to have increased cardiovascular risk and increased liver lipid (production) levels.
NAFLD is a risk factor for ischemic stroke, fibrosis, hypertension, chronic kidney disease, atrial fibrillation, myocardial infarction, ischemic stroke and death from cardiovascular causes. Liver cancer develops in NASH in the absence of cirrhosis in 45% in the cases.
The outcome in the broadest possible terms is a composite of gene X gene, environment X environment and gene X environment interactions. Identification of the genome I148M PNPLA3 variant as the major common genetic determinant of NAFLD. Other moderate effect size variants are TM6SF2, MBOAT7 and GCKR.
Current gold standard of liver biopsy for diagnosis will be an impractical one. Liver enzymes are often within the normal range even in advanced disease. Non-invasive tools to stage and grade the severity of metabolic liver disease have been developed. MRI and MRE techniques have the best performance. Blood-based biomarkers for staging and grading NAFLD are particularly attractive for population level disease screening.
Also Read:Obesity and Non-alcoholic Fatty Liver Disease
Current guidelines recommend lifestyle intervention with diet modulation and physical activity as first line management for NAFLD/NASH. Physical activity reduces liver fat even if there is no weight reduction. Weight loss, through exercise or diet, was shown to be the most effective way to reduce liver fat and help NASH and fibrosis remission. 150 to 200 min/week in 3 to 5 sessions of moderate intensity aerobic physical activity or resistance training is beneficial. Aerobic exercise may be more effective.
NAFLD might benefit from a moderate to low-carbohydrate diet and low-fat diet. Mediterranean diet also shows reduction of NASH induced inflammation and liver fibrosis in 6-weeks. 500-1000 kcal/week less than the daily diet, 7-10% weight loss, a low to moderate fat and moderate to high carbohydrate diet or a low carbohydrate ketogenic or high protein diet. Avoid all fructose-containing beverages and food. Vitamin-E is beneficial. Omega-3 fatty acid is useful for hypertriglyceridemia in patients with NAFLD. Coffee and tea appear to have beneficial effects.
Insulin sensitizers reduce insulin resistance in those with NAFLD. Bariatric surgery is an effective method for obese and diabetic individuals.

Article by Dr. Vadivel Kumaran, MD(GEN.MED).,DM(MED. GASTRO)
Consultant Medical Gastroenterologist & Hepatologist
Kauvery Hospital

