INTRODUCTION:
Pasteurella sp have general characteristics being non-motile, facultative anaerobic and Gram-negative coccobacilli. These are mostly found in the oral cavity and the gastrointestinal tract of certain animals which transmit the infections. Cats and dogs being the highest carriage rates, at 70% to 90% and 20% to 50%, respectively. Usually, infections by Pasteurella spp. in humans is more common in the context of an animal bite leading to a skin and soft tissue infection (SSTI). Pasteurella spp rarely causes Infective endocarditis, and because of its rarity there is both diagnostic with therapeutic dilemmas. Here we present a case of Infective Endocarditis caused by Pasteurella.
CASE REPORT :
This 19-year-old female with no known co-morbidities initially presented to outside hospital with history of fever for 5 days associated with breathlessness and vomiting. On evaluation CT chest done showed Bilateral pleural effusion with ascites. Initially she was evaluated for tropical fever which was negative. Blood cultures showed Pasteurella Multocida, hence treated with doxycycline. Initial echo done showed Normal LV function. She was shifted to our hospital for further management with NIV support.

MANAGEMENT:
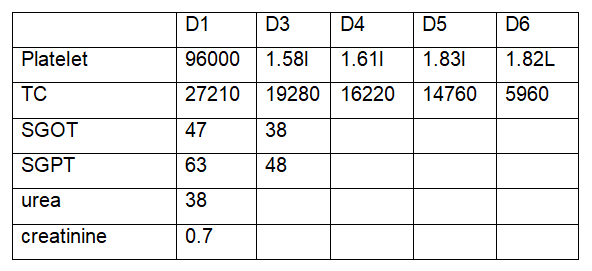
On arrival she was conscious, oriented, haemodynamically stable requiring 10l of 02 support. Cultures were repeated in view of persistent fever spikes. Antibiotics were continued (Inj.Meropenem and Inj.Doxy). Initially she was on NIV, later she was tapered off to HFNC.
On Day 2 of admission, she developed rashes over right palm (Janeway lesions) Echo done showed mobile vegetation attached to Anterior mitral leaflet (17*12 mm) posterior mitral leaflet (8*6) and primary chordae with intermittent moderate MR. Surgery was considered when there was increasing MR/ Vegetation increasing in size / persistent fever in spite of antibiotics. Antibiotic Inj. Vancomycin were also added. Repeat ECHO done showed vegetation attached to Anterior mitral leaflet (19*7 mm) posterior mitral leaflet (9*8). Trans esophageal echo done also confirmed the same findings. Hence, she was taken up for valve replacement surgery.
DISCUSSION:
Pasteurella spp which is found worldwide is a component of normal flora of upper respiratory tract of fowl and mammals especially Pasteurella multocida. Pasteurella can lead to various diseases in animals, including fowl cholera in poultry, shipping fever in cattle (with P. multocida contributing to secondary infections after parainfluenza), hemorrhagic septicemia in cattle and lambs, fibrinous pneumonia in cattle, snuffles in rabbits, and other localized infections.
While most human infections are caused by dog or cat bites, non-bite transmission has also been reported, including infections from animal licks. Cats and dogs licking non-intact skin on distant areas have resulted in infections in nearby prosthetic joints, such as total knee or hip replacements. In some cases, kissing animals has been identified as the source of Pasteurella infections. Indirect transmission through fomites has been suggested as well, with cases of infants suffering severe P. multocida infections linked to pet saliva on pacifiers or a sibling’s finger. A recent review indicated that non-bite transmission is more common in older individuals and those with comorbidities, often leading to more life-threatening infections than those caused by bites. This is similar to our case where the patient and their family denies any direct contact with animals.
Infections caused by P. multocida can be categorized into the following.
–Soft tissue infections, such as cellulitis, can occur after animal bites or scratches; these bites and scratches may also lead to abscesses and necrotizing soft tissue infections.
–Bone and joint infections. P. multocida can cause septic arthritis and/or osteomyelitis.
–Respiratory infections, typically in individuals with chronic pulmonary disease.
P.multocida can lead to a range of upper and lower respiratory tract infections, including glossitis, pharyngitis, sinusitis, otitis media, mastoiditis, epiglottitis, tracheobronchitis, pneumonia, empyema, and lung abscesses. Most patients with P. multocida respiratory infections have preexisting lung conditions, such as chronic obstructive pulmonary disease or chronic bronchitis.
–Severe invasive infections, often not associated with animal bites, including meningitis, intra-abdominal infections, endocarditis, or ocular infections.
The rarity of Pasteurella-induced infective endocarditis (IE) is reflected in the limited literature, with only around 48 cases reported to date. While gram-positive organisms are the most common causes of IE, infections caused by gram-negative bacteria (primarily E. coli and Pseudomonas) account for less than 10% of cases. As a result, managing the even rarer gram-negative Pasteurella-induced IE is challenging in the absence of established clinical guidelines.
Treatment of Pasteurella endocarditis is challenging and mainly based on anecdotal evidence, as the available data primarily comes from case reports. However, there is a general consensus that aggressive antibiotic therapy is essential for all patients. Broad-spectrum cephalosporins, piperacillin-tazobactam, and ampicillin-sulbactam have been used, with some cases also treated with ciprofloxacin. In our case, the organism was sensitive to meropenem, vancomycin, and linezolid, but resistant to penicillin and cephalosporins. A 6-week course of antibiotics is considered optimal. Surgical intervention is necessary for cases involving severe valvular dysfunction, antibiotic failure, or an aortic root abscess. In our case, the lack of improvement after 5 days of medical management led us to consider surgery, which proved to be successful.
CONCLUSION:
Pasteurella-induced IE is rare and highly morbid with an aggressive clinical course. High index of suspicion and early diagnosis, especially in immunocompromised patients, are warranted because the disease is potentially life threatening, yet is a readily treatable infection.
REFERENCES:
- Giordano A, Dincman T, Clyburn BE, et al. Clinical Features and Outcomes of Pasteurella multocida Infection. Medicine (Baltimore) 2015; 94:e1285.
- Donnio PY, Lerestif-Gautier AL, Avril JL. Characterization of Pasteurella spp. strains isolated from human infections. J Comp Pathol 2004; 130:137.
- Wilson BA, Ho M. Pasteurella multocida: from zoonosis to cellular microbiology. Clin Microbiol Rev 2013; 26:631.
- Owen CR, Buker EO, Bell JF, Jellison WL. Pasteurella multocida in animals’ mouths. Rocky Mt Med J 1968; 65:45.
- Acha PN, Szyfres B. Zoonoses and Communicable Diseases Common To Man and Animals, 3rd Ed, Pan American Health Organization, Washington, DC 2001. Vol 1, p.199.
- Nettles RE, Sexton DJ. Pasteurella multocida prosthetic valve endocarditis: case report and review. Clin Infect Dis 1997; 25:920.
- Mahmoud M, El Kortbi K, Abdalla MI, Habib S. Rare but Fatal Pasteurella multocida Infective Endocarditis: A Case Report and Literature Review. Cureus 2022; 14:e22950.
 Dr. Ramapriya
Dr. Ramapriya
Critical Care
Kauvery Hospital, Chennai



