Coronary artery disease is the foremost cause of death in many countries and hence, its early diagnosis is concerned as a major healthcare priority. Coronary artery calcium scoring using either electron beam computed tomography or multislice computed tomography has been applied to provide an early CAD diagnosis in clinical practice.
Most of the coronary events occur in the territory of coronary arteries do not demonstrate prior high-grade stenosis. Although atherosclerotic plaque is invariably present in an acute coronary event, significant stenosis is not necessarily seen. The complications of atherosclerotic plaque like erosion / rupture and followed by thrombus formation are important events leading to acute coronary syndrome. Plaque composition, hemodynamics, endothelial function, and blood coagulability like factors may influence and leads to hemodynamically significant events. There is a strong relation between the risk of a coronary event and extent of coronary plaque. Atherosclerosis is the only disease process associated with calcification of the coronary arteries, hence the degree of coronary calcification detected by CT is predictive of the overall burden.
Calcium scoring is a simple test and it hardly take not more than 5 minutes. ECG leads are placed on the patient. To determine the location of the heart, scout image is obtained. A prospective ECG-gated scan is then obtained from the level of the carina through the bottom of the heart with 3-mm slice thickness. To get an accurate calcium score, calcium within the coronary arteries must be distinguished from calcification of other parts of the heart, especially the aortic or mitral valve. Mitral annular calcification may be present adjacent to the circumflex artery, whereas aortic annular calcification may be present adjacent to the left anterior descending artery. The effective radiation dose from a calcium scoring is in the range of 1.0 to 1.5 mSv.
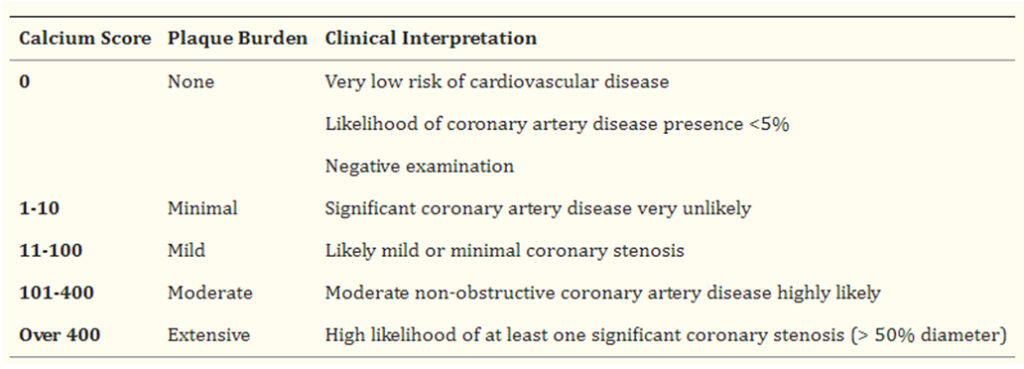
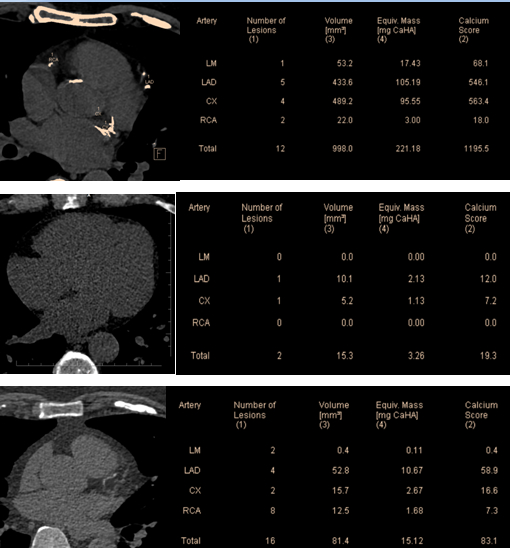
Automated program is used to compute a calcium score once CT examination is done. The Agatston method has been traditionally used to score the amount of coronary calcium with CT. For each focus of calcified coronary plaque, area and maximum attenuation are measured. Then assign an attenuation cofactor to each plaque based on CT attenuation measured in Hounsfield units. The cofactor is designated as 1 for 131 – 200 HU, 2 for 201 – 300 HU, 3 for 301 – 400 HU, and 4 for >400 HU. To achieve a calcium score, the area of each plaque is multiplied by the appropriate attenuation cofactor. The scores of each individual plaques in all the vessels are generally summed to obtain Agatston calcium score for risk analysis. Scores are generally divided into normal, mildly elevated, moderately elevated, or severely elevated. Mildly elevated coronary calcium scores are present without significant coronary stenosis. Calcified plaque is frequently associated with positive remodeling, resulting in no significant narrowing of the internal vessel lumen. As the level of coronary calcium increases, the risk of significant stenosis is higher, but there is no linear correlation. Mild to Moderately elevated calcium scores may be associated with normal coronary vessels on angiography. Patients with severely elevated calcium scores are more likely to have a significant stenosis, but these patients are also the most challenging to study with CT coronary angiography because of artifact from calcification. Calcium scoring is generally used to assess patient risk for a cardiac event, not to detect the presence of coronary stenosis.
Density factor:
- 130-199 HU: 1
- 200-299 HU: 2
- 300-399 HU: 3
- 400+ HU: 4
 Dr. Shabna Jasmin K
Dr. Shabna Jasmin K
Radiology Resident
Kauvery Hospital