Priya Philip1,*, AN. Aswin2, Andrew C. Fenn2, AN. Vaidhyswaran3
1Registrar, Department of Radiation Oncology, Kauvery Hospital, Chennai, India
2Consultant, Department of Radiation Oncology, Kauvery Hospital, Chennai, India
3Senior Consultant and Director, Department of Radiation Oncology, Kauvery Hospital, Chennai, India
*Correspondence: priyaphilipk@gmail.com
ABSTRACT
Hepatocellular carcinoma is the most common malignancy of liver and third leading cause of cancer death. Most of the patients present in advanced stage. Portal vein tumour thrombosis is a common complication of HCC which leads to a median survival of only 2.7 months. Patients with PVTT are ineligible for liver transplantation and there is no survival benefit. PVTT is a contraindication for TACE due to chance for ischaemia and liver necrosis. Systemic management using multikinase inhibitors like Sorafenib or Regorafenib improve overall survival (OS) by 2 months only. SBRT delivers high dose of radiation in few fractions (one to five fractions). A 65 years old gentleman who is a known case of chronic hepatitis C viral infection and previous history of hepatocellular carcinoma in left lobe of liver in 2016 presented with a new lesion in the right lobe of liver. Right branch of portal vein along with its superior and inferior branches were thrombosed. Patient was taken up for radiotherapy by SBRT technique -40Gy in five fractions. Follow up PET CT revealed excellent response. Patient is being taken up for liver transplantation. Our case study shows the role of radiation as a bridging technique before the definitive treatment in HCC.
INTRODUCTION
Hepatocellular carcinoma is the fifth most common cancer in the world and the most common primary malignancy of liver [1]. It is the third leading cause of cancer death worldwide. 80% of patients are diagnosed in the advanced condition when it is in the unresectable stage. If the patient presents in early stage, the treatment is hepatectomy if the liver functions are normal. Liver transplantation is considered if the patient with HCC meets Milan Criteria-single lesion ≤5cm, or ≤3 lesions ≤3cm; no extrahepatic lesions ;no macrovascular invasions. In patients where a curative surgery is not possible, local treatment modalities like radiofrequency ablation (RFA), transcatheter arterial chemo-embolisation and radiation therapy are used. Macrovascularinvasion (MVI) is common in advanced HCC. Tumor cells invade the portal vein, hepatic veins or inferior venacava in the liver. Portal vein tumour thrombosis (PVTT) is the most common type of MVI, incidence ranging from 44 to 62.2% [2]. About 10-60% patients with HCC have portal vein thrombosis at diagnosis [2]. PVTT is a poor prognostic factor and the median survival is only 2.7-4months [3]. Patients with PVTT are ineligible for liver transplantation and there is no survival benefit. PVTT is a contraindication for TACE due to chance for ischaemia and liver necrosis. Systemic management using multikinase inhibitors like Sorafenib or Regorafenib improve overall survival (OS) by 2 months only[3]. Treating the PVTT by radiotherapy gives promising results as a down staging or bridging therapy for surgery.
SBRT delivers high dose of radiation in few fractions (one to five fractions). High biological effective dose (BED) compared to the conventional fractionation radiation course and shorter treatment time ensures safe and effective management of PVTT. SBRT is aimed at shrinking the tumour thrombus and maintain portal venous flow, so that patient can undergo curative procedure like resection or TACE. We present a case recently encountered and managed with SBRT.
CASE REPORT
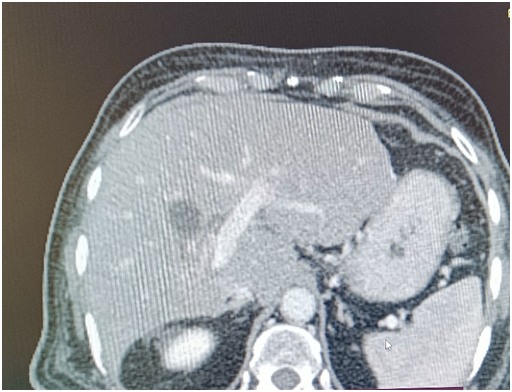
We had a 65 years old gentleman who is a known case of chronic hepatitis C viral infection and chronic liver disease. He had other co-existing conditions such as diabetes mellitus, hypertension and ischaemic heart disease. He had a history of hepatocellular carcinoma in 2016 which was managed by laparoscopic left lateral segmentectomy. He was disease free since then and in remission with HCV. Recently he developed abdominal pain, fever and backache for about a month duration. On evaluation he was found to have elevated GGT values and Alpha feto protein (AFP-33,732 ng/ml). Imaging with MRI and MRCP revealed a focal lesion of size 8.2×5.6×9.1cm in the segment VI of liver. There was enhancement with contrast and washout in delayed phase. The characteristics were suggestive of hepatocellular carcinoma. Triple phase CT abdomen showed an ill-defined enhancing lesion involving segments V, VI and VII of liver showing enhancement in arterial and portal phase with hypodense areas suggestive of necrosis. The lesion measures 10.3×5.8cms. Right branch of portal vein and its superior and inferior branches thrombosed. (figure-1A,1B,1C)

Figure-1A

Figure-1B

Figure 1-C
He was started on oral therapy with Lenvatinib. He was planned for radiotherapy to the portal vein thrombosis by SBRT technique and thus making him eligible for liver transplantation.
Patient was immobilized with a thermoplastic device and planning CT scans were taken in arterial and portal venous phases. Different phases of respiration were also considered. The images were co-registered with the treatment planning system. The target area and organs at risk were contoured. (Figure-2) Using 10MV FFF photons, a total dose of 40Gy in 5 fractions were delivered to the planning target volume (PTV) using SBRT technique. (figure 3A,B,C). The patient tolerated the treatment well and did not develop any post procedural complications.
Figure 2-Target volume and organs at risk contoured


Figure 3A – Radiation dose distribution(100%)

Figure 3 -B-isodose volume -100%

Figure 3 -C-50% isodose distribution
PET CT after 1.5 months showed excellent response. The portal vein and branches were normal. (Figure 4-A,B) The patient is being planned for liver transplantation. Our case study shows the role of radiation as a bridging technique before the definitive treatment in HCC.
Figure 4-A

Figure 4-B
DISCUSSION
Hepatocellular carcinoma is the most common malignancy of liver and third leading cause of cancer death. Most of the patients present in advanced stage. Portal vein tumour thrombosis is a common complication of HCC, which leads to a median survival of only 2.7 months if left untreated. The presence of PVTT pose a contraindication for local therapies like transarterial chemo embolization and surgery. Pre-operative SBRT offers greater chance of resectability and low toxicity. SBRT as a bridging technique prior to liver transplantation showed a complete pathological response rate of 27-63% [3].
Cheng et al. proposed tumor thrombus types system-Type I, tumor thrombi locating at the segmental branches (second order branches of portal vein or above; Type II, tumor thrombi extending to involve the right or left portal vein (first-order branches); Type III, the main portal vein trunk involved; Type IV, the superior mesenteric vein or inferior vena cava invaded. The classification is useful for initial assessment and decide treatment strategies.
Even though HCC is a radiosensitive tumour, radiotherapy is not considered as the first line treatment as HCC occurs in a background of chronic liver disease and poor tolerance of liver to radiation. There is difficulty in localizing primary tumour also. SBRT is a new radiotherapy technology used for precise delivery of a high dose of radiation to an extracranial target within the body, using either a single dose or a small number of fractions. Que JY et al[8]recommended SBRT can be delivered safely to huge HCC and achieved a substantial tumor regression and survival, suggesting this technique may be considered a salvage treatment of HCC and PVTT. Sanuki N et al. [9] reported that SBRT was critical to improve local control or potential cure in liver lesions not amenable to first-line surgical resection or radio frequency ablation.
A multi-centreclinical trial done in USA showed that for the non-resectable HCC patients treated with SBRT, overall freedom from local progression was 63% at a median follow-up of 12.9 months, the median time to local progression was 6.3 months, the 1- and 2-years overall survival rates were 87% and 55%, respectively [10]. The local and regional recurrence remain the major causes of SBRT failure; further studies of combination of SBRT and other treatment modalities need to be carried out.
CONCLUSION
Radiotherapy using SBRT technique is an effective method of treating portal vein tumour thrombosis in hepatocellular carcinoma which would be otherwise unresectable or not eligible for local therapies, thus facilitating further curative or definitive management strategies.
REFERENCES
1. Comparison of stereotactic body radiation therapy with and without sorafenib as treatment for hepatocellular carcinoma with portal vein tumor thrombosis – Jenny Que, Hung-Chang Wu, Chia-Hui Lin, Chung-I Huang, Li-ChingLi, Chung-Han Ho
2. Stereotactic body radiotherapy basedtreatment for hepatocellular carcinoma with extensive portal vein tumorthrombosis-Shui, Yu, Ren, Guo, Xu, Ma, Zhang, Wu, Yongjie Wei Xiaoqiu Yinglu Jing Tao Bicheng Jianjun Li, Hu, Shen, Bai, Liang Wei1, Qinghai Qiongge Li Xueli Tingboand Qichun
3. Preoperative Stereotactic Body Radiotherapy to Portal Vein Tumour Thrombus in Hepatocellular Carcinoma: Clinical and Pathological Analysis
4. Noriko Kishi1*, Naoyuki Kanayama1, Takero Hirata1, Shingo Ohira1, Kentaro Wada1,Yoshifumi Kawaguchi1, Koji Konishi1, Shigenori Nagata2, Shin-ichi Nakatsuka2,Shigeru Marubashi3, Akira Tomokuni3, Hiroshi Wada3, Shogo Kobayashi3,4, Yasuhiko Tomita2&TerukiTeshim
5. Zhang ZM, Lai EC, Zhang C, et al. The strategies for treating primary hepatocellular carcinoma with portal vein tumor thrombus. Int J Surg. 2015; 20:8–16.
6. Chan SL, Chong CC, Chan AW, Poon DM, Chok KS. Management of hepatocellular carcinoma with portal vein tumor thrombosis: Review and update at 2016. World J Gastroenterol. 2016;22(32):7289–300.
7. Zhong JH, Peng NF, You XM, et al. Tumor stage and primary treatment of hepatocellular carcinoma at a large tertiary hospital in China: A real-world study. Oncotarget. 2017;8(11):18296–302.
8. J.Y. Que, L.C. Lin, K.L. Lin, et al., The efficacy of stereotactic body radiation therapy on huge hepatocellular carcinoma unsuitable for other local modalties, Radiat. Oncol. 9 (1) (2014) 120.
9. N. Sanuki, A. Takeda, E. Kunieda, Role of stereotactic body radiation therapy for hepatocellular carcinoma, World J. Gastroenterol. 20 (12) (2014) 3100e3111
10. R.A. Ibarra, D. Rojas, L. Snyder, et al., Multicenter results of stereotactic body radiotherapy (SBRT) for non-resectable primary liver tumors, ActaOncol. 51 (5) (2012) 575e583



 Dr. Priya Philip
Dr. Priya Philip Dr. A. N. Aswin
Dr. A. N. Aswin Dr. Andrew C Fenn
Dr. Andrew C Fenn Dr. A. N. Vaidhyswaran
Dr. A. N. Vaidhyswaran