
An Informed Perspective on Causes, Diagnosis, Treatment, and Advanced Surgical Techniques
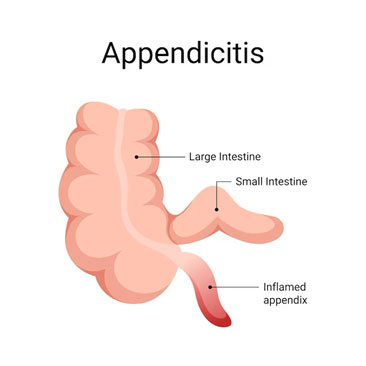
Acute appendicitis stands as one of the most frequently encountered surgical emergencies globally. It is a condition marked by inflammation and infection of the appendix — a narrow, finger-shaped organ attached to the large intestine. Though its physiological purpose remains a subject of ongoing research, appendicitis is a definitive medical urgency that, if untreated, can lead to severe and potentially life-threatening complications. Fortunately, modern advancements in medical science, particularly in diagnostic and surgical methods, have transformed the way this condition is managed, ensuring safer interventions and expedited recovery.
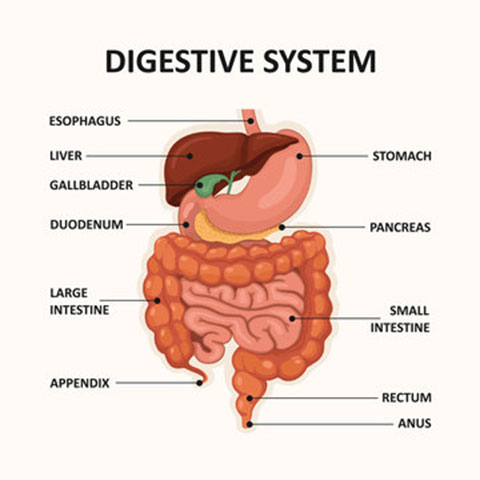
Anatomical Insights: The Appendix
The appendix is often regarded as a vestigial organ, yet recent studies suggest it may play a modest role in supporting gut health and immune function. Despite this, its susceptibility to blockage and infection makes it a common source of medical concern. Appendicitis, characterized by acute inflammation of the appendix, demands swift diagnosis and intervention to mitigate risks.
Etiology of Acute Appendicitis
The onset of appendicitis is typically precipitated by obstruction of the appendiceal lumen, which results in bacterial overgrowth, swelling, and subsequent infection. Common causes include:
- Fecaliths: Hardened stool deposits obstructing the lumen.
- Lymphoid Hyperplasia: Swelling triggered by infections or inflammatory processes.
- Foreign Bodies: Rare blockage caused by ingested objects such as seeds.
- Parasitic Infections: Organisms like Ascaris lumbricoides or Enterobius vermicularis may occasionally cause appendicitis.
These factors collectively contribute to increased intraluminal pressure, reduced blood flow, and localized infection, culminating in the hallmark symptoms of appendicitis.
Clinical Presentation: Recognizing Appendicitis
The symptoms of acute appendicitis often begin subtly but progress rapidly. Recognizing the following signs is crucial for timely medical attention:
- Abdominal Pain: Initially diffuse around the umbilical region, the discomfort migrates to the lower right quadrant as the inflammation intensifies.
- Nausea and Vomiting: These symptoms are frequently reported alongside the abdominal pain.
- Fever: Mild pyrexia often accompanies the body’s inflammatory response.
- Loss of Appetite: A notable decrease in hunger is a common complaint.
- Digestive Disturbances: Occasional instances of diarrhea or constipation may occur, though they are less prevalent.
Diagnostic Approach: Combining Expertise and Technology
The diagnosis of appendicitis requires a meticulous blend of clinical evaluation, laboratory investigations, and imaging studies.
Clinical Examination
During a physical examination, healthcare providers assess for localized tenderness, particularly in the right lower quadrant, along with signs like rebound tenderness and guarding. Special diagnostic maneuvers, such as Rovsing’s sign or the psoas test, may further solidify the clinical suspicion.
Laboratory Analysis
Blood tests often reveal elevated white blood cell counts and inflammatory markers, such as C-reactive protein. While these findings provide supportive evidence, they are not definitive and must be corroborated with imaging results.
Imaging Modalities
- Ultrasound: A non-invasive, radiation-free option, especially suitable for paediatric or pregnant patients.
- Computed Tomography (CT): Renowned for its high accuracy, CT imaging provides detailed visualization of the appendix and surrounding tissues.
- Magnetic Resonance Imaging (MRI): Though less commonly utilized, MRI offers an alternative for patients requiring avoidance of radiation exposure.
Surgical Intervention: A Modern Perspective
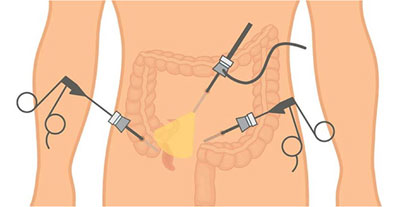
Surgical removal of the appendix, or appendectomy, remains the gold standard treatment for acute appendicitis. The approach to surgery has evolved significantly, with minimally invasive techniques such as laparoscopic and robotic appendectomy emerging as preferred options.
Laparoscopic Appendectomy
Widely recognized for its efficiency and patient-centered benefits, laparoscopic appendectomy involves the insertion of a small camera and specialized instruments through tiny incisions. Key advantages include:
- Minimized postoperative scarring, leading to superior cosmetic outcomes.
- Reduced postoperative pain and discomfort.
- Accelerated recovery, allowing quicker return to daily activities.
- Lower incidence of wound infections and other complications.
Robotic Appendectomy
Robotic-assisted surgery represents the pinnacle of precision and technological advancement in surgical care. Employing state-of-the-art robotics, this technique offers unparalleled accuracy and control. Advantages include:
- Even smaller incisions, enhancing aesthetic results and reducing tissue trauma.
- Improved dexterity during complex or challenging cases.
- Minimized blood loss and optimized surgical outcomes.
- Enhanced patient recovery times with fewer complications.

Postoperative Recovery and Care
Following an appendectomy, patients typically experience a smooth recovery. Pain management, proper wound care, and adherence to medical guidance ensure favourable outcomes. Most individuals resume their normal routines within a few weeks of the procedure.
Complications of Neglecting Appendicitis
Delaying treatment for appendicitis can lead to severe complications, such as:
- Appendiceal Rupture: The inflamed appendix may burst, causing widespread infection and peritonitis.
- Abscess Formation: Localized pus accumulation may necessitate drainage procedures.
- Sepsis: A systemic infection resulting from untreated appendicitis can be life-threatening.
Conclusion
Acute appendicitis serves as a reminder of the importance of timely medical intervention and the transformative power of modern surgical techniques. With options like laparoscopic and robotic appendectomy, patients benefit from precise, minimally invasive procedures that ensure rapid healing and reduced risks. By recognizing the symptoms and seeking immediate care, individuals can mitigate complications and embrace a swift recovery, bolstering their health and well-being.

Dr. Joyner Abraham M
Consultant Minimal Access & Robotic Surgery,
Kauvery Hospital, Chennai
A Second Sunrise: A Story of Gratitude
Life has a strange way of reminding us how precious each moment truly is. What began as an ordinary day turned into one of the most testing chapters of our lives — and also the most humbling.
My wife had been feeling unwell for a few days — a nagging pain in her stomach, which we assumed was something minor. Like most people, we brushed it off. Maybe it was gas, maybe acidity, or perhaps just stress. But as the day went on, her discomfort escalated to unbearable pain, and we knew something was not right.
We rushed to Kauvery Hospital, clinging to hope and silently praying it wasn’t something serious. That’s where we met Dr. Kavitha, a calm and compassionate presence who wasted no time. After examining my wife and going through the necessary scans, she delivered news that made our hearts sink — a ruptured appendix.
The word “ruptured” rang in my ears like an alarm bell. I had always heard about appendicitis, but never imagined the pain and danger it brings when left undetected. Dr. Kavitha explained it with clarity and urgency. The rupture had already begun releasing infection into her abdomen, and immediate surgery was the only way to save her.
The symptoms were like UTI but clinical examination and CT findings were a ruptured appendix which was sealed throughout by the omentum.
(Dr Joyner explained very clearly later that the adhesions were with the bladder and hence the symptoms were related to painful urination.)
Without hesitation, the team at Kauvery swung into action. It was then that we were introduced to Dr. Joyner, the surgeon who would perform the complex operation. His confidence and reassuring words gave us a thread of strength to hold on to. In that moment, we had no choice but to trust — to surrender to their skill, their experience, and above all, their humanity.
The surgery began, and those few hours felt like an eternity. Every tick of the clock echoed in my chest. But finally, we received the news: The operation was successful.
I still remember the first time I saw her after surgery. Though tired, her face had a calmness that filled me with gratitude — she was safe. The next three days in recovery felt like watching the sunrise after a terrifying storm. Each passing hour brought improvement, and soon, she was walking again, eating, smiling — returning to herself.
Today, as I hold her hand, I realize how close we came to the edge. It’s easy to take health, time, and even love for granted, until you come face-to-face with the possibility of loss.
To Dr. Kavitha, thank you for your sharp eye, timely action, and kindness. You didn’t just diagnose the problem — you gave us clarity when we were lost in confusion.
To Dr. Joyner, thank you for your skilled hands and steady heart. You didn’t just operate — you gave my wife another chance at life, and gave me my world back.
To the entire team at Kauvery Hospital, thank you for the care, attention, and empathy you extended to us during those crucial days. You all were not just professionals, but healers in the truest sense.
This experience has taught me the power of gratitude. It reminded me that even in moments of fear, there are people who become our pillars. And to anyone reading this — if you love someone, don’t wait for a crisis to show it. Life can change in an instant.
For us, that change came with a scar, but it also came with a miracle. And for that, we will always be grateful.

