Bladder Control Problems in Elderly with Parkinsonism
Parkinson’s disease is a neurodegenerative disorder, involving the dopaminergic neurons. Here, due to a deficiency in dopamine in the nigrostriatal pathway, there will be tremors, slow movement (bradykinesia) and skeletal rigidity. The duration of the disease is an important factor for the presentation of bladder symptoms, as are the stage and progression of Parkinson’s disease.

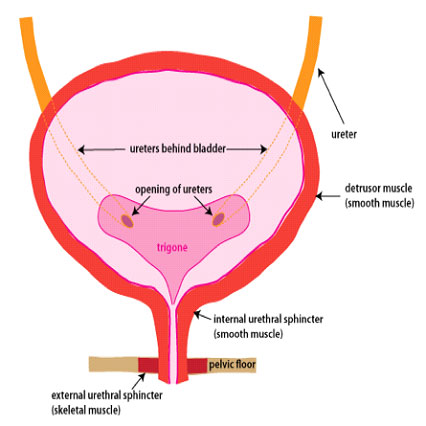
Normally the urinary bladder, is a muscular storage organ for urine, which empties as per the patient’s will and situation. As simple as the statement maybe, there is involvement of several pathways signalling, coordinating and finally emptying the bladder or exerting control. There are also a set of valve mechanisms involved which help us with controlling the urine outflow at will, which is called the striated or external urethral sphincter. Another set of valve mechanism called the internal urethral sphincter which is located around the neck of the urinary bladder, is also called the involuntary sphincter or which cannot be controlled at the patient’s will. There are 2 phases of the urinary bladder function; storage and emptying. During storage phase, the bladder is relaxed and the sphincters or valves are in a state of contraction to help maintain urinary continence or to prevent urine leakage. The second phase is emptying (micturition), where the goal is to completely empty the bladder, so that the bladder muscle contracts and the sphincters relax to help achieve this. Disruption of this normalcy can lead to various bladder-related symptoms.
A set of symptoms called lower urinary tract symptoms (LUTS) are seen to happen due to involvement of the bladder or anywhere below it in the outflow tract. Storage symptoms are increased urinary frequency, night-time urination (nocturia) and urinary urgency. Others can be urinary incontinence. Emptying phase symptoms are straining to pass urine, slow or poor urinary stream, difficulty initiating urinary flow (hesitancy), feeling of incomplete emptying of the bladder and interruption in urinary flow.
After having learned the basics of bladder mechanics and the symptoms associated with the lower urinary tract, we can look into the symptom complexes associated with Parkinson’s disease. Lower urinary tract dysfunction can occur in 35 to 70 percent of patients! It takes about 5 years from the time of onset of the disease for initial symptoms, subject to disease stage and duration. The most common symptoms which our patients see are, nocturia (86%), frequency (71%) and urinary urgency (68%). So, as seen with this statistic, storage urinary symptoms are the most frequently encountered symptoms followed by obstructive urinary symptoms and thereafter a mix of both. The external sphincter is seen to exhibit a delayed relaxation when wanting to void. Bladder muscle overactivity is often seen. There also may be a poor contraction of the bladder muscle or rarely, an acontractile bladder.
We have to remember that in an ageing population there will be coexistence of symptoms due to enlargement of the prostrate. These require thorough evaluation to identify the causative issue and cause-directed therapy. Surgical treatment for enlarged prostate maybe done, since the chances of an acontractile external sphincter are extremely rare. Ideally, these patients need urodynamic evaluation as poor bladder contractions with ineffective relaxation of the external sphincter, will be a cause for poor post-operative results.
Quality of life can be directly impacted due to nocturia and increased urinary frequency. We need to understand that the patients with Parkinson’s disease will have certain limitations, which unfortunately we need to take up with extreme consideration; such as slowed movements which affect the ability to reach the restroom on time to relieve themselves, hand tremors which increase difficulty with self-catheterisation if needed, etc.
The continuous treatment for PD in terms of medication is to be followed rigorously to help control some of the symptoms. Meanwhile for bladder-associated disturbances, the use of anti-cholinergic medication which help to bring down bladder overactivity and alpha-blockers as needed maybe added. Other than medication, certain invasive therapies maybe used such as deep brain stimulation, peripheral nerve neuromodulation (tibial nerve) or even injection of botulinum toxin which will help in ameliorating the symptoms, but should only be considered under expert advice.


