Why Is Fasting Required Before Anesthesia?
Whenever patients are planned for surgery or any procedure under anesthesia, we the anesthesiologists request you to fast and in emergency scenarios we would like to make a note about your last meal time and details. Why is this one of the safety concerns for the patient and what will the impact be if there is a compromise while following fasting guidelines is the key message of this article.

Other than the operation theatre, certain procedures where intravenous sedation is planned are endoscopy, colonoscopy, bronchoscopy, MRI scan (when patient has claustrophobia and anxiousness or difficulty lying down flat), CT guided biopsy, radiotherapy for paediatric age group and angiogram procedures. For planned elective surgeries and procedures, patients are seen earlier for fitness and evaluated. The query about fasting arises – why do they have to fast and when will they be allowed to resume a normal diet after the surgery? This is asked especially when patients are children, elderly, people with diabetic conditions, people who can’t tolerate fasting i.e., prone for hypoglycaemia, headache, giddiness, syncope, gastritis, gastroesophageal reflux disease, etc. Pregnancy is also a condition where fasting becomes challenging.
With any anesthesia, there is a risk for aspiration. Even though the procedure is under local anesthesia, it’s better to have an empty stomach, as anxiousness and fear of pain can induce vomiting which will be a hindrance during the procedure. If there is undigested food in the stomach, it will cause aspiration of food into the lungs. It happens because there is loss of protective airway reflex under anesthesia. The muscle tone is relaxed, so when food contents ascend there is no control and the food particles enter the lungs. In simple terms, generally our body has some sort of control when vomiting sensation is experienced and you are aware of it; for some amount of time, you can hold that reflex and that control is lost under anesthesia. Hence it leads to aspiration and respiratory infection (pneumonia) and illness which can lead to prolonged critical care observation and deterioration in lung function. We cannot bring out the aspirated contents from lungs. The aim of fasting is to prevent aspiration. This is applicable only for planned and elective procedures. In emergency situations, we take preventive measures like only general anesthesia with gastric tube suction to take out the stomach contents (as life-saving procedures need to be taken without any delay). If the procedure can be timed, fasting is strictly advised and followed.
How can we prevent the adverse effects of fasting? Yes, we do take precautions and administer preventive medications to help the patients overcome the unpleasant fasting hours. Children are taken up earlier in the morning schedule so that the fasting hours are avoided. Getting admitted 4 to 6 hours prior to any procedure is advised – at least 3 hours if the plan is day care. This helps to start the patient on intravenous fluids to maintain hydration, which in turn prevents low sugar levels and low blood pressure. There are chances of dehydration which will lead to an increase in heart rate, low blood pressure, giddiness and syncopal attack. All of these can be prevented by maintaining hydration. Proton pump inhibitors are given to prevent acid reflux in an empty stomach. Antiemetics are given thirty to sixty minutes prior to the procedure. Anaesthetic agents have the potential side effects of inducing nausea and vomiting. Anti-anxiety drugs are given for anxious patients according to their age and weight, keeping their other co-existing illnesses in consideration, as anxiousness causes sleep disturbance, increased heart rate & blood pressure.
The patient is kept nil per mouth minimum of 3 hours post-surgery for both regional and general anesthesia. For intravenous anesthesia, oral intake is started once the patient is awake and alert enough to swallow food particles. If it’s a local anesthesia and nerve block procedure with no sedatives administrated, orals can be started at once. When it is a major surgery and abdominal surgery, the protocol differs and we wait for clearance from the operating surgeon.
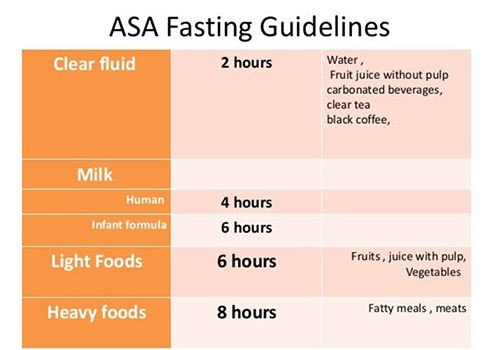
The tabular column gives you the list of contents and allowable hours of consumption before surgery. Clear water is the clear liquid suggested to be on safer side. No aerated drinks or juices with pulp; any liquid with cream contents formula, milk substances are not considered as clear liquids. Any meat and cheese, ghee, fried junk food containing fatty substances takes time to digest. Hence it is taken into account for 8 hours. Bland and staple food, formula milk intake is allowed for 6 hours prior to the procedure. Breast milk should be stopped 4 hours prior. People with chronic diabetes and obesity and pregnant patients have tendency for delayed gastric emptying. When the patient is induced for normal delivery, she is kept on nil per oral as the labor progresses, by following the guidelines in order to avoid aspiration risk, as there can be a change of plan and need for surgery anytime.
I would like to emphasise again that the fasting guidelines are for your own safety. When it is an elective procedure, it’s ideal to follow guidelines for fasting. If the fasting time is not suitable or is a hindrance for your physical well-being, you can always plan a light meal 6 hours before the surgery according to your taste buds. A bland, oil-less and balanced diet is the best as it is easier to digest and keeps the stomach guarded i.e., idly, bread, biscuits with your cup of coffee or tea. We would like you to be on an empty stomach before we put you on anesthetic sleep.
ASA – American Society of Anesthesiologists

Dr. K. Mahalakshmi
Consultant Anaesthesiologist
Kauvery Hospital, Chennai

