
What Is Mobility?
Mobility refers to the ability to move the body freely and independently. This includes walking, transferring from bed to chair, using a wheelchair, walker, or cane, and performing coordinated movements involving both the upper and lower body. It encompasses the ability to move various joints and muscles to perform essential body movements.
Activities of Daily Living (ADLs) and Mobility
Mobility plays a vital role in performing basic activities of daily living (ADLs), such as:
- Self-feeding
- Dressing and grooming (e.g., combing hair)
- Carrying objects
- Walking and standing
- Sitting and transitioning between sitting and standing
- Climbing stairs and squatting
- Picking up objects from the floor
- Floor sitting (e.g., cross-legged sitting)
Why Is Mobility Important?
Mobility is essential for maintaining independence, self-care, and an improved quality of life. Being able to move without depending on others allows individuals to participate actively in personal, social, and community life.
“Mobility = Freedom of Movement”
Factors Affecting Mobility
Mobility can be impaired due to various factors, including:
- Injuries and pain
- Aging and age-related changes
- Post-surgical conditions, especially orthopaedic surgeries like total knee replacement (TKR), etc.
- Neurological conditions such as stroke, Parkinson’s disease, spinal cord injuries, etc.
- Cardiopulmonary surgeries and related conditions
- Chronic conditions like obesity, diabetic neuropathy, or limb amputation
- Chronic illness
Reduced mobility can significantly affect a person’s life by:
- Decreasing independence in daily activities
- Lowering the overall quality of life
- Increasing the risk of falls and related injuries
- Leading to social isolation and emotional distress
Maintaining or restoring mobility through physiotherapy, regular exercise therapy, and medical intervention is crucial for ensuring long-term health, confidence, and autonomy.
Physiotherapist Goal
Physiotherapists play a vital role in enhancing mobility, restoring lost movement, and improving flexibility. They are highly skilled in assessing and treating movement dysfunctions and are capable of developing personalized treatment plans tailored to exercise therapy for each patient’s needs and goals.
Specific exercise training programs must be planned by a physiotherapist after taking into consideration the health status of the patient, age, sex, and other clinical conditions such as the presence of other pathologies (i.e., cancer, obesity, diabetes, neurodegenerative disorders, etc.) or specific disabilities, and functional ability and fitness level.
Assessing mobility and flexibility is crucial for identifying functional limitations and creating an effective treatment strategy. Physiotherapists utilize a range of tests and measurements, including range of motion and muscle strength assessments, to evaluate a patient’s physical capabilities.
Loss of mobility can have serious negative impacts on an individual’s quality of life. Inability to move freely and without pain may lead to depression, weight gain, and other adverse health outcomes. It can also diminish self-confidence and a sense of self-worth.
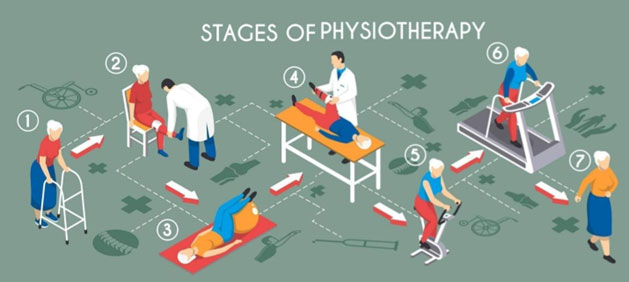
Physiotherapy Techniques to Restore Mobility
Physiotherapists utilize a variety of techniques to help restore mobility, reduce pain, and improve overall function. These include:
1. Therapeutic Exercise Therapy Like Stretching, Range of Motion (ROM), Strengthening Exercise, Balance and Coordination Exercise, Endurance Training and Functional Exercise and Manual Therapy
Therapeutic exercise refers to a carefully planned and structured set of physical activities designed to restore and improve physical function, strength, flexibility, endurance, balance, and overall mobility. These exercises are prescribed and supervised by physiotherapists based on the patient’s specific condition, limitations, and rehabilitation goals.
Goals of Therapeutic Exercise:
- Improve or restore range of motion
- Increase muscle strength and endurance
- Enhance flexibility and joint mobility
- Promote balance and coordination
- Reduce pain and muscle tension
- Prevent re-injury and promote long-term functional independence
2. Physical Modalities
Physiotherapists may use electrotherapy modalities to reduce pain and inflammation, and facilitate mobility.
3. Patient Education and Advice
Education on ergonomics, posture, and pain management is an essential component. Patients are also advised on injury prevention and strategies to maintain mobility after recovery.
4. Regular Follow-Up
Ongoing assessment allows the physiotherapist to monitor progress and adjust the treatment plan as needed, ensuring optimal recovery and sustained mobility.
5. Gait Training
Gait analysis helps identify abnormal walking patterns. Based on this, physiotherapists provide corrective strategies and interventions to improve walking efficiency.
6. Mobility Aids and Assistive Devices
To support recovery and safe movement, physiotherapists may recommend the use of mobility aids such as walkers, tripods, elbow crutches, or axillary crutches, depending on the patient’s needs.
Goal of Physiotherapy
The primary aim is to help patients regain their independence and confidence by improving their ability to move safely and effectively. Through comprehensive assessment and customized interventions, physiotherapists work to restore optimal physical function and quality of life.
Case Study 1
I would like to share this particular patient’s history: A 30-year-old female walked into our physiotherapy department. She had a history of shoulder pain that was radiating all the way down to her arm and hand. She told me she had already been taking medication to relieve the pain, but 10 days had passed and nothing worked. By this time, she was not able to lift her arm, which was extremely painful. The moment I took her history; I started to assess her and found the reason to be purely musculoskeletal.
I began our treatment exercise therapy and electrotherapy and functional-based physiotherapy program; she was 50% cured in the first visit. She felt the magic truly happen, and she left for home happily. On the same evening, this patient sent me a text stating that she was able to switch on the fan. Imagine a 30-year-old woman expressing her gratitude for just a fan operating chore. Just think about the kind of disability that she was facing. Think about the relief she received.
Case Study 2:
A Second Chance at Life Through Physiotherapy
Patient Profile
A 45-year-old female was admitted to the Intensive Care Unit (ICU) with septic shock affecting her right lower limb. She underwent emergency abdominal surgery and was managed in the ICU for stabilization. Once her vital signs and overall clinical condition improved, the physiotherapy team was consulted to initiate early mobilization.
Initial Condition
At the time of the first physiotherapy session, the patient was profoundly weak. She was unable to lift her hands or legs and was incapable of performing basic movements such as bed mobility or side turning. Despite her physical limitations, the patient demonstrated motivation and trust in the physiotherapy process.
Physiotherapy Intervention in the ICU
Early physiotherapy focused on passive joint mobilization and passive bed mobility training, with the goals of preventing pressure sores, minimizing pulmonary complications, maintaining joint integrity, and instilling confidence in the patient. Once clinically stable, she was discharged from the hospital with a structured home-based physiotherapy plan.
Post-Discharge Physiotherapy Program
Physiotherapy continued at home with a focus on exercise therapy aimed at improving mobility, neuromuscular coordination, proprioception, balance, and muscle strength. Within 3 to 4 weeks, the patient regained basic mobility, including the ability to sit up in bed and ambulate short distances with assistance.
Functional Progression
Over time, she progressed to independent toileting and bathing. Indoor ambulation became unassisted, and under the supervision of the physiotherapist, the physiotherapy program shifted toward stair-climbing and outdoor gait training. Approximately two months post-surgery, the patient was able to leave her home for the first time. She expressed mixed emotions of joy and fear but gradually gained confidence through daily walking practice under supervision and with family support.
Return to Pre-Morbid Activities
As her functional status and confidence improved, the patient expressed a desire to return to the gym, an activity she enjoyed prior to her illness. At this stage, she continued to experience low stamina and high levels of perceived exertion. The physiotherapy plan was accordingly adjusted to include endurance and cardiovascular training.
Outcome
Following two additional months of structured physiotherapy focused on stamina
and endurance, the patient successfully regained full functional mobility. She resumed gym activities and began participating in outdoor trips, including traveling and visiting temples (Kashi, Kedarnath Temple). She expressed immense gratitude to her physiotherapist, stating, “This is my second life. You helped me transition from being completely dependent to fully independent.”
Conclusion
This case highlights the pivotal role of physiotherapy in restoring mobility, function, and quality of life following critical illness. Through early intervention, patient-centered approach, and consistent support, physiotherapists empower patients not only to recover but to reclaim their independence and confidence.

Ms E. Savithra, BPT., MPT (Sports)
Physiotherapist
Kauvery Hospital, Chennai

