
Minimally invasive brain and spine surgery is something many of us hope for when surgery becomes necessary. Since the brain and spine are such delicate and important parts of the body, it’s best to use surgical methods that cause the least damage to healthy tissues. That’s what minimally invasive surgery aims to do — solve the problem while protecting as much of the normal body as possible.
Let’s delve into some details and clarifications about these surgeries, why they matter and how they are done.
This type of surgery is not about doing something fancy or just trying new technology. It’s about what the patient needs. And the reasons are clear:
- These surgeries are possible thanks to modern tools.
- The technology needed is available to us.
- Surgeons need the right training and skills to perform them.
- Most importantly, the surgeon knows the needs and will take the decision on the basis of the lesion and the accessibility to the lesion to protect the patient’s safety and health. That decision shows maturity and experience.
Minimally Invasive Brain Surgery – How It Works
In brain surgery, getting access to the problem area is the first step. This is usually done in two ways:
- Through the top of the skull
- Through the base of the skull, often by going through the nose
Going through the nose helps reach deep parts of the brain. Using endoscopes (tiny cameras) and microscopes, doctors can see clearly and perform the surgery without needing large openings.
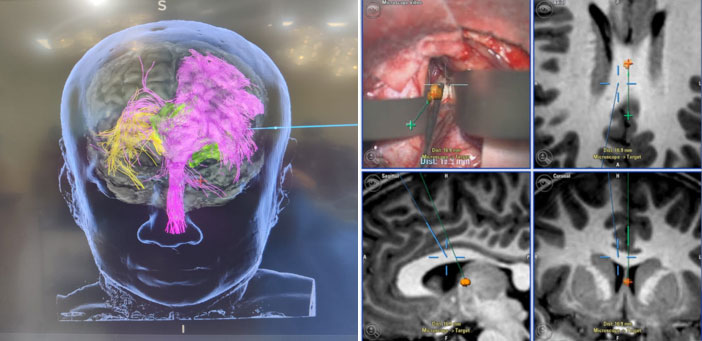
These tools help magnify the area so surgeons can work with better precision. In fact, with 3D viewing, they can see small details clearly and safely remove problem areas while protecting healthy brain tissue.
For brain tumors near the surface, we use other tools like:
- Neuronavigation – a GPS-like system that guides the surgeon to the exact spot.
- Exoscopes – advanced cameras that allow better visualization.
- MR Tractography – an advanced MRI technique that maps important brain pathways (like those for movement or speech), helping surgeons avoid critical areas and reduce the risk of damage.

These help make much smaller cuts in the skin and skull, which means quicker recovery and less pain.
For deeper brain issues, like bleeding (hemorrhagic stroke), we can make a small hole in the skull and guide an endoscope inside. This allows us to remove clots or pressure without needing a large operation.
Minimally Invasive Spine Surgery – A Safer Approach
Similar to brain surgery, spine surgery can also be done in a minimally invasive way. The spine has natural spaces that allow small instruments and cameras – endoscopes to enter.
There are multiple endoscope techniques that we use like Unilateral Biportal Endoscopic Technique.
Using these, surgeons can fix issues in the spine — like disc problems or nerve compression — through very small cuts.
We also use:
- Navigation systems like the O-arm to plan and guide the surgery
- Tubular retractors, which are small, tube-like tools that help reach the problem area without cutting much muscle or bone
- Robotic tools and even AI (artificial intelligence) to improve accuracy
But sometimes, using an endoscope may not be possible. In such cases, other minimally invasive tools can still help the surgeon do the job with minimal damage.


Why Minimally Invasive Surgery Matters
Minimally invasive surgery is not just about using small tools. It’s about:
- Causing less damage to healthy tissue
- Making smaller cuts, means less pain, faster recovery, and shorter hospital stays
- Using the latest technology wisely
- Making decisions that are best for the patient, not just what’s new or exciting
Final Thoughts
Minimally invasive brain and spine surgery is not just a new trend — it’s a much-needed improvement in how we treat serious conditions.
It means doing less harm while fixing the real problem.
It requires skill, training, the right tools — and the wisdom to know when to use them.
Sometimes, the best choice is to go ahead with minimally invasive surgery. But other times, the safest option might be a more traditional approach. A good surgeon always keeps the patient’s well-being as the first priority.
So, minimalism in surgery isn’t just about being modern — it’s about being thoughtful, careful, and focused on the best outcome for the patient.

Why This Approach Matters
Minimally invasive surgery is about more than just small cuts. It’s about:
- Less pain after surgery
- Minimal scar
- Lesser damage to tissues
- Faster healing and recovery
- Lower chances of infection
- Shorter hospital stays
- Better overall outcomes for the patient
It also requires proper planning, the right equipment, and a well-trained team. Most importantly, it requires the surgeon to know when this approach is right, and when it’s not — because safety and long-term results are what matter most.

Dr Shyam Sundar
Senior Consultant Neurosurgeon,
Kauvery Hospital, Chennai

