A complex neonatal presentation requiring Ladd’s procedure: A case report
Gayathri1, Gowdham P2, Savitha V N3
1Staff Nurse, NICU, Kauvery Hospital, Marathahalli, Bangalore
2Senior Nurse Educator, Kauvery Hospital, Marathahalli, Bangalore
3DNS, Kauvery Hospital, Marathahalli, Bangalore
Abstract
Neonatal morbidity often results from combined respiratory, metabolic, and gastrointestinal pathologies. While meconium aspiration syndrome (MAS) is a common cause of early respiratory distress in term neonates, metabolic complications including polycythaemia and hypoglycaemia frequently complicate the clinical course in low-birth-weight infants. Neonatal hyperbilirubinemia remains a ubiquitous concern, and structural gastrointestinal anomalies such as midgut malrotation are surgical emergencies requiring prompt intervention. Recognizing these conditions early, and managing them in a multidisciplinary fashion, is critical to avoid morbidity and mortality.
Key words: Ladd’s procedure; Meconium Aspiration Syndrome (MAS); Neonatal Hyperbilirubinemia
Case Presentation
Patient Profile
- Gestational Age: Early Term (37+1 weeks)
- Sex: Male
- Birth Weight:46 kg (Appropriate for Gestational Age)
- Mode of Delivery: LSCS for thick meconium-stained amniotic fluid and previous LSCS
- Place and Time of Birth: Kauvery Hospital, Marathahalli, 27/10/2025 at 10:46 AM
- Apgar Scores: 8/10 at 1 min, 9/10 at 5 min
Maternal History
A 27-year-old G2P1L1 mother under regular antenatal care. Fully immunized; VDRL, HIV, HBsAg non-reactive; blood group A positive. No significant antenatal complications.
Initial Course
At birth, the neonate had good respiratory effort, tolerated early feeding, and passed small amount of meconium within 24 hr.
Clinical Findings and Management
1. Meconium Aspiration Syndrome (Respiratory)
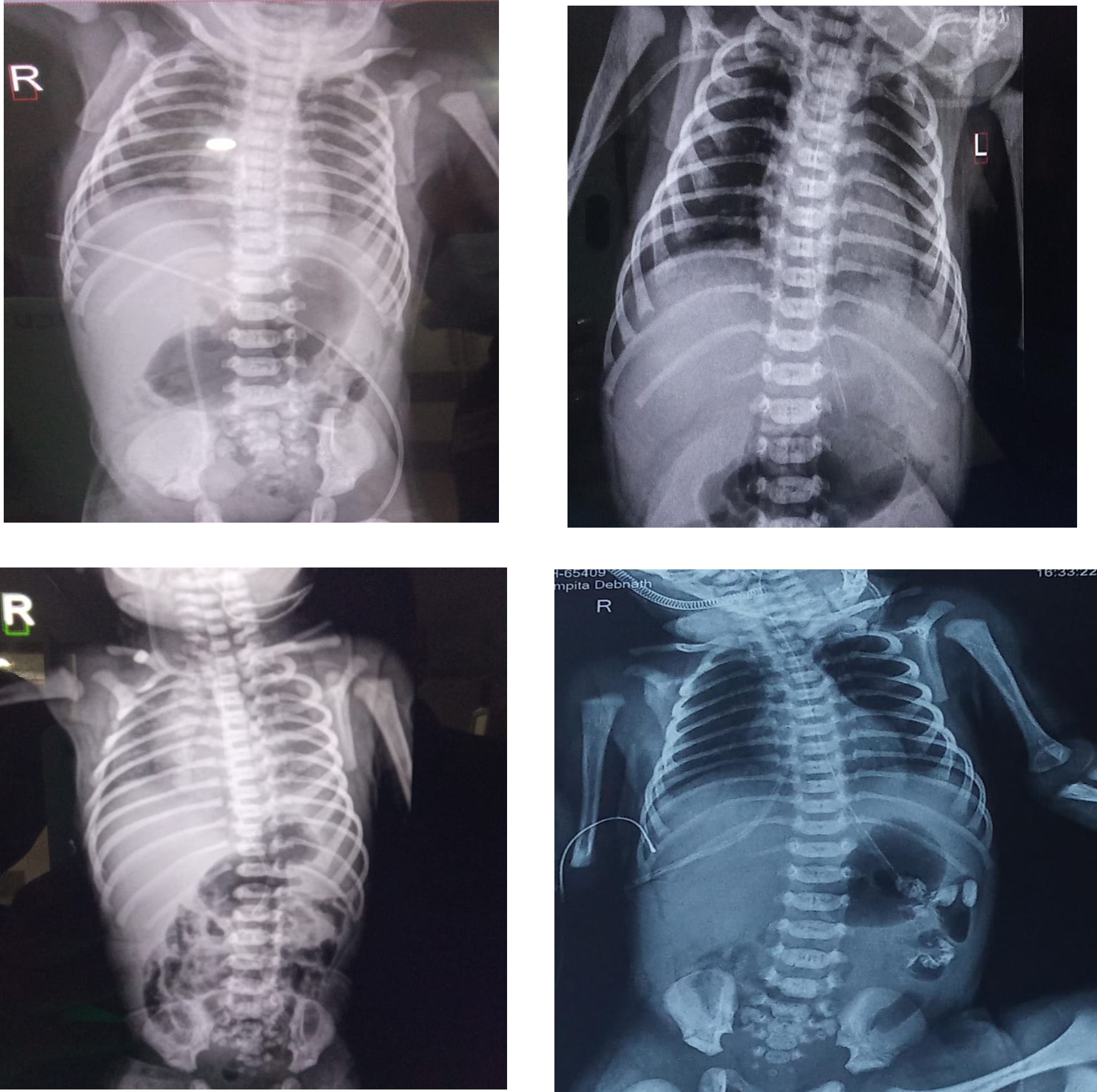
At approximately 12 hours of life, the neonate developed respiratory distress. Chest X-ray revealed heterogeneous pulmonary opacities without hyperinflation. High-flow nasal cannula (HFNC) support was initiated at 5 L/min with FiO₂ 25 %. HFNC continued for 7 days, then weaned to low-flow support and finally to room air by day 9. Intravenous AUGMENTIN and Amikacin were administered; blood culture was sent.
2. Polycythaemia & Asymptomatic hypoglycaemia
Routine glucose monitoring revealed persistent asymptomatic hypoglycaemia (lowest GRBS 26 mg/dL), prompting NICU transfer by 6 hours of life and infusion of 10 % dextrose. Haematological workup showed polycythaemia with Hb 26 g/dL and PCV 75 %. With IV fluids and careful monitoring, Hb stabilized to 22.9 g/dL and PCV to 68.4 %. Progressive feeds were attempted but later withheld due to gastrointestinal symptoms.
3. Neonatal Hyperbilirubinemia
At 24 hours, serum bilirubin was 9.4 mg/dL. Double surface phototherapy was provided for 12 hours with successful reduction in levels.
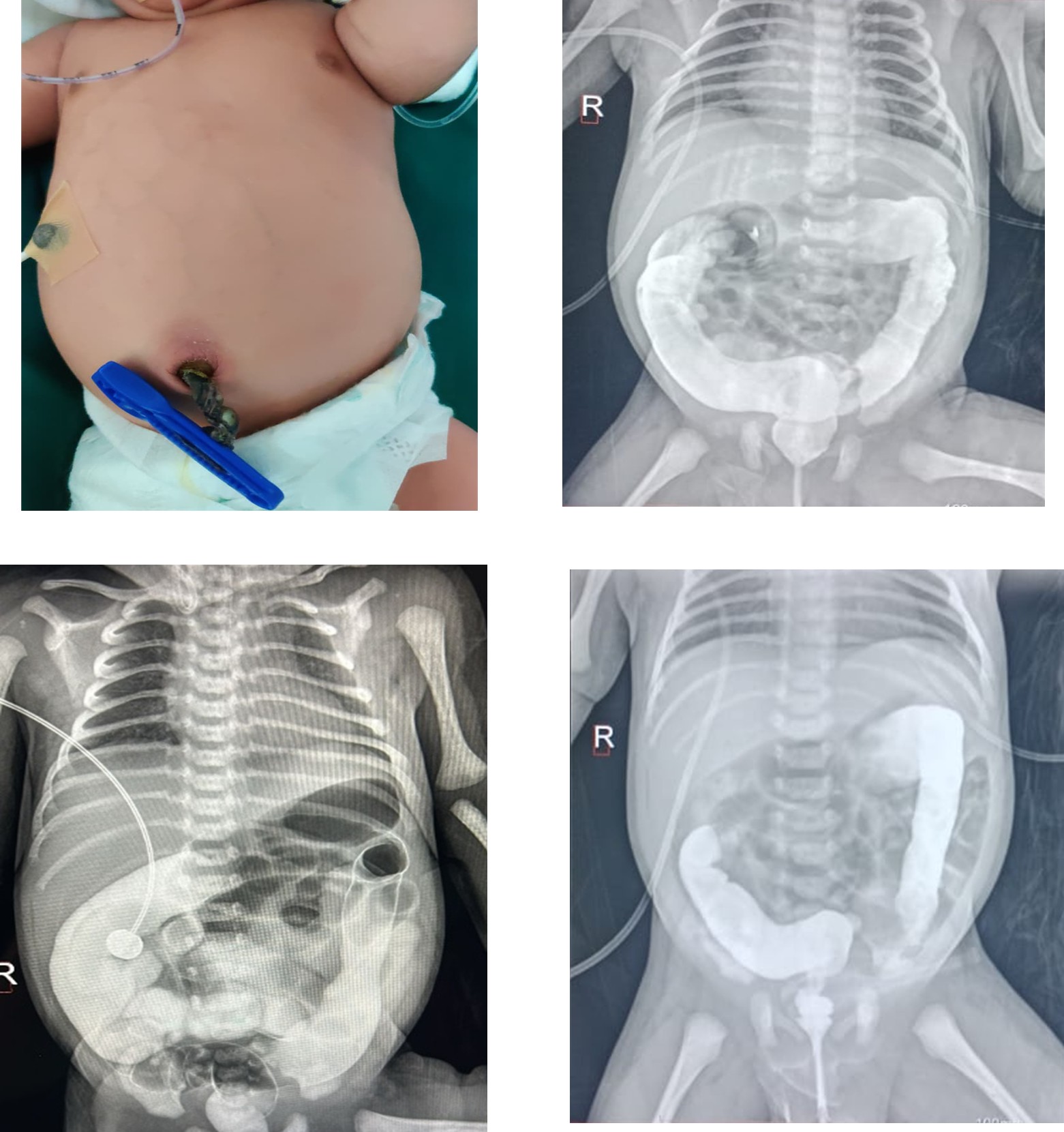
4. Midgut Malrotation (Surgical Condition)
As feeds advanced, the baby developed tachypnea and bile-stained gastric aspirates. From 30 hours, feeds were withheld (NPO). Sepsis markers were elevated (CRP 4.1 mg/dL) and antibiotics were escalated, but bilious aspirates persisted. Abdominal ultrasonography suggested malrotation, and a contrast study confirmed obstruction. On day 4 of life, emergency exploratory laparotomy was performed. Midgut malrotation was identified; de rotation and Ladd’s procedure were successfully completed. Postoperatively, the baby remained NPO for 3 days and received glucose infusion and amino acid nutrition. Enteral feeds were restarted on postoperative day 3 and advanced gradually to full feeds by day 12.
5. Sepsis Assessment
Initial sepsis screen was positive, but blood cultures showed no growth. Metronidazole was given post-operatively for 7 days. A peripherally inserted central catheter (PICC) was removed after 8 days without complications.
6. Cardiovascular Evaluation
2D echocardiography demonstrated a small patent ductus arteriosus (PDA) 1.8 mm, which closed spontaneously by day 3. The neonate remained hemodynamically stable without inotrope support.
7. Diaper Dermatitis
Diaper rash developed and was treated with a zinc-oxide barrier, antifungal ointment (clotrimazole 1 %), and a brief course of hydrocortisone 1 % cream, with significant improvement.
Investigations and Screening
- Blood Group: A positive
- Thyroid Profile: TSH sample sent on day 3 of life
- CCHD Screening: Normal SpO₂ readings (98 % RUL, 99 % RLL)
- Red Reflex: Bilaterally present
Anthropometry at Discharge
- Weight: 2.42 kg
- Length: 48 cm
- Head Circumference: 33 cm
Immunization & Medications
- Hepatitis B: 27/10/2025
- BCG & OPV: 09/11/2025
- Vitamin K: Given
- Supplementation: Ultra-D3 (400 IU) 1 ml daily until 1 year; A-Z drops 0.5 ml daily for 1 month
Discharge Advice
Parents received comprehensive counselling on:
- Thermal protection
- Exclusive breastfeeding guidance (every 2–3 hours)
- Cord and skin care
- Jaundice monitoring
- Hearing screening, routine immunization
- Diaper rash management and hygiene
Outcome
The baby tolerated feeds, remained hemodynamically stable, and showed appropriate weight gain. Multidisciplinary care enabled successful transition from NICU to discharge in good condition.
Discussion
This case demonstrates a rare and complex convergence of respiratory, metabolic, and surgical conditions in an early-term neonate, emphasizing the importance of continuous clinical vigilance and a multidisciplinary approach in neonatal intensive care.
Meconium Aspiration Syndrome and Respiratory Outcome
Meconium aspiration syndrome (MAS) remains a significant cause of respiratory distress in term and near-term neonates, particularly in deliveries complicated by thick meconium-stained amniotic fluid. In this neonate, respiratory distress developed within the first 12 hours of life, consistent with delayed presentation of MAS. The chest radiograph showing heterogeneous opacities without hyperinflation suggested moderate disease severity. Early initiation of non-invasive respiratory support with HFNC prevented the need for mechanical ventilation, thereby reducing the risk of ventilator-associated lung injury and chronic lung disease. Gradual weaning based on clinical stability highlights the importance of individualized respiratory management protocols.
Polycythaemia and Asymptomatic hypoglycaemia
Polycythaemia in neonates can be associated with placental insufficiency, perinatal stress, or intrauterine hypoxia. Increased blood viscosity may impair tissue perfusion and contribute to metabolic complications such as hypoglycaemia. In this case, persistent asymptomatic hypoglycaemia despite enteral feeding prompted early NICU admission and intravenous glucose therapy. Prompt recognition and correction were essential to prevent potential neurological injury. Conservative management with fluids resulted in gradual improvement of haematocrit levels, avoiding the need for partial exchange transfusion. This underscores the importance of routine glucose monitoring in low-birthweight and at-risk neonates.
Neonatal Hyperbilirubinemia
Neonatal hyperbilirubinemia is frequently observed in early-term and low-birth-weight infants due to hepatic immaturity and increased red cell turnover, which may be exacerbated by polycythaemia. Early detection and timely initiation of phototherapy in this neonate successfully prevented progression to severe hyperbilirubinemia and bilirubin-induced neurologic dysfunction. Regular bilirubin surveillance remains a cornerstone of neonatal care, particularly in infants with additional risk factors.
Diagnostic Challenges in Midgut Malrotation
Midgut malrotation often presents with non-specific symptoms in the neonatal period and may be masked by concurrent systemic illnesses such as sepsis or respiratory distress. In this case, the initial emphasis on respiratory and metabolic stabilization had the potential to delay recognition of the underlying surgical pathology. However, the persistence of bilious gastric aspirates associated with progressive abdominal distension, even during nil per oral status, served as a critical red-flag sign. Early imaging with abdominal ultrasonography followed by contrast study enabled timely diagnosis and intervention. This reinforces that bilious aspirates with abdominal distension in neonates should be treated as a surgical emergency until proven otherwise.
Surgical
Management and Nutritional Support
Ladd’s procedure remains the definitive treatment for midgut malrotation and is most effective when performed before the onset of volvulus and bowel ischemia. Early surgical intervention in this neonate resulted in preservation of bowel integrity and favourable postoperative recovery. Postoperative nutritional management with glucose infusion and amino acid supplementation played a vital role in maintaining metabolic stability and promoting healing until enteral feeds could be safely resumed. Gradual feed advancement minimized the risk of feed intolerance and necrotizing enterocolitis.
Sepsis Evaluation and Antibiotic Stewardship
The presence of elevated inflammatory markers with negative blood cultures reflects the diagnostic challenge of neonatal sepsis. In postoperative and critically ill neonates, empirical antibiotic coverage is often necessary; however, timely de-escalation based on culture results and clinical response is equally important to prevent antimicrobial resistance. Removal of invasive lines such as PICC at the earliest appropriate time further reduced infection risk.
Cardiovascular and Hemodynamic Stability
The incidental finding of a small patent ductus arteriosus that closed spontaneously highlights the importance of echocardiographic evaluation in neonates with respiratory distress. Continuous monitoring ensured early detection of potential hemodynamic compromise, though no intervention was required in this case.
Nursing Care and Family centred Approach
Comprehensive nursing care was integral throughout the hospital course, including respiratory monitoring, glucose surveillance, fluid management, postoperative care, skin integrity maintenance, and parental education. Management of diaper dermatitis prevented secondary infection and discomfort, contributing to overall neonatal wellbeing. Lactation counselling and discharge education empowered caregivers to continue appropriate care at home.
Clinical Implications and Learning Points
This case underscores several key clinical lessons:
- The need for high suspicion of surgical pathology in neonates with persistent bilious aspirates,
- The importance of early metabolic stabilization in preventing neurological sequelae.
- The value of coordinated multidisciplinary care in managing complex neonatal conditions.
Early-term infants, though often perceived as low risk, may present with significant morbidity requiring advanced neonatal and surgical support.
Key learning points
- Persistent bilious aspirates and feeding intolerance in neonates should prompt immediate imaging for surgical pathology.
- Early recognition of polycythaemia and hypoglycaemia and timely metabolic support prevent neurologic sequelae.
- Multidisciplinary teamwork between neonatology, paediatric surgery, nursing, and allied care significantly improves outcomes.
- Detailed nursing protocols for respiratory support, fluid management, pain control, wound and diaper care are essential for optimal recovery.
Conclusion
This case highlights the importance of vigilant monitoring, early diagnosis, and prompt multidisciplinary intervention in complex neonatal presentations. Early surgical management of malrotation via Ladd’s procedure, along with supportive medical and nursing care, contributed to an excellent clinical outcome.
References
- Fan W, Walker WA. Meconium aspiration syndrome: Pathophysiology and prevention. J Pediatr. 2020;216:10–15.
- Garg M, Devaskar SU. Glucose metabolism in the newborn. Pediatr Clin North Am. 2015;62(2):377–388.
- Black VD, Lubchenco LO, Koops BL, et al. Neonatal polycythemia: Clinical and hematologic consequences. Pediatrics. 1985;75(6):1039–1045.
- Maisels MJ, McDonagh AF. Phototherapy for neonatal jaundice. N Engl J Med. 2008;358(9):920–928.
- Dennery PA, Seidman DS, Stevenson DK. Neonatal hyperbilirubinemia. N Engl J Med. 2001;344(8):581–590.
- Neonatal Resuscitation Program (NRP). Textbook of Neonatal Resuscitation. 8th ed. American Academy of Pediatrics; 2021.
- Torres AM, Ziegler MM. Malrotation of the intestine. World J Surg. 1993;17(3):326–331.
- Snyder CL. Intestinal malrotation. Semin Pediatr Surg. 2003;12(4):229–236.
- Kliegman RM, St Geme JW, Blum NJ, et al. Nelson Textbook of Pediatrics. 21st ed. Philadelphia: Elsevier; 2020.
- Grosfeld JL, O’Neill JA, Fonkalsrud EW, Coran AG. Pediatric Surgery. 7th ed. Philadelphia: Elsevier; 2012.