Effect of diet and lifestyle modifications on non-pharmacological HbA1c reduction in a new onset diabetes pre-renal transplant donors: A pilot study
Umamaheswari. K
Manager, Clinical Nutrition and Dietetics, Kauvery Hospital, Hosur, Tamil Nadu
Abstract
Dietitians play a critical role in the reduction of HbA1c levels through effective dietary interventions within a month. They assess individual nutritional needs and develop personalized meal plans focused on controlling carbohydrate intake, promoting balanced nutrition, and minimizing glycaemic fluctuations. Dietitians educate patients on portion control, the importance of low-glycaemic index foods, and the elimination of unhealthy dietary habits. By fostering adherence to these dietary modifications, they enable patients to achieve better blood glucose management and noticeable HbA1c reduction within a short time frame. Their expertise in nutritional counselling complements lifestyle changes, ensuring sustainable diabetes control and reducing the risk of complications.
Key words: HbA1c levels; Organ transplantation; Amsterdam Forum
Introduction
Pre-transplant donor health is crucial to ensure the safety and success of organ transplantation. Glycaemic control plays a significant role in reducing risks during and after donation. Poor glycaemic control, as indicated by elevated fasting blood sugar, postprandial blood sugar, and HbA1c levels, can lead to complications such as delayed wound healing, increased risk of infections, and other metabolic issues that could compromise the donor’s health post-donation. Additionally, maintaining optimal glycaemic levels ensures better organ function and reduces long-term risks for both the donor and recipient. The prevalence of diabetes and prediabetes among potential donors poses significant challenges for transplantation. Candidates with fasting blood sugar levels above 126 mg/dL or postprandial levels above 200 mg/dL are considered diabetic, while those in the pre-diabetic range (postprandial levels between 140-199 mg/dL and HbA1c levels between 5.7%-6.4%) require medical clearance and regular monitoring.
“The Amsterdam Forum has set forth a comprehensive list of medical criteria that is now used internationally in the evaluation of potential kidney donors; although a diagnosis of diabetes precludes donation, the presence of prediabetes does not necessarily render a potential donor unacceptable.” [1,2]
Case Presentation
Pre-Transplant Donor with New-Onset Diabetes
This case involves a pre-transplant donor who has successfully completed the initial medical work-up required for kidney donation. During the evaluation process, the nephrologist identified new-onset diabetes in the donor, which necessitates immediate attention and management before proceeding with the transplant. Diabetes, being a metabolic disorder, can significantly impact the donor’s overall health and the success of the transplant. Therefore, a referral was made to the dietitian for comprehensive nutritional intervention and monitoring over a period of 4-6 weeks. The primary goal of this intervention is to optimize the donor’s metabolic health, stabilize blood glucose levels, and prepare them for the transplant procedure. The dietitian’s role involves designing a personalized nutritional plan, monitoring key health parameters such as fasting blood sugar, postprandial blood sugar, and HbA1c levels, and implementing lifestyle modifications aimed at improving insulin sensitivity and overall health. This pre-transplant phase is critical to ensure the donor’s readiness for surgery and to minimize potential complications. The dietitian will work closely with the nephrologist and other healthcare professionals to provide a holistic approach to diabetes management, focusing on dietary adjustments, physical activity, and regular follow-ups. This case highlights the importance of multidisciplinary collaboration in addressing newly diagnosed diabetes in pre-transplant donors to ensure optimal outcomes for both the donor and the recipient. For pre-transplant donors identified with new-onset diabetes, it is crucial to implement a structured nutrition intervention and monitoring plan before the transplant. Here’s an elaboration of the process over the 4–6-week period:
1. Initial Assessment
Medical History Review: Evaluate the donor’s medical history, including blood sugar levels (Fasting, Postprandial, and HbA1C) as per guidelines
Pre transplant Work up Donor’s investigations
| Biochemical parameters | Donor 1 | Donor 2 | Donor 3 | Donor 4 |
|---|---|---|---|---|
| Haemoglobin | 12.7 | 14.5 | 13.5 | 12.3 |
| TLC | 9000 | 11470 | 7280 | 5900 |
| PLT | 3.29 | 2.6 | 3.41 | 2.26 |
| BUN | 21 | 28.3 | 32 | |
| Creatinine | 0.7 | 1.0 | 1.1 | 0.6 |
| Sodium | 143 | 138 | 140 | 138 |
| Potassium | 4.8 | 4.2 | 4.0 | 4.11 |
| FBS | 111 | 161 | 101 | 115 |
| PPBS | 101 | 150 | 130 | 136 |
| HbA1c | 6.6 | 7.4 | 6.7 | 6.6 |
| Triglycerides | 85 | 332 | 116 | 83 |
| Total Cholesterol | 160 | 204 | 196 | 138 |
2. Dietary Assessment
Analyse current eating habits, caloric intake nutrient deficiencies and diet recall.
Diet recall of Donors
| Meal Timings | Menu | Quantity |
|---|---|---|
| Early Morning (7-8 am) | Tea/coffee with half sugar | 200ml |
| Breakfast (9-10 am) | Idli/ Dosa/ Pongal/ Ragi ball/ Rice Chutney / sambar | 3-4 / ½ cup -1 cup |
| Midmorning (11-12pm) | Tea/ coffee with sugar | 200ml |
| Lunch (2-3 pm) | Rice/ Ragi ball/ Rice Bath sambar/ fish curry/ chicken curry vegetables (weekly thrice) | 1 cup 1 cup ½ cup |
| Evening (5-6 pm) | Biscuit /Bonda/ Bajji (weekly thrice) Tea/ coffee with sugar | 2-3 150ml |
| Dinner (9-10pm) | Ragi ball/ Rice bath/ Dosa/ Chapati Chutney / sambar | 3-4 / 1 cup ½ cup |
Approximate Nutritive Value
| Nutrients | Values (%) |
|---|---|
| Energy (kcal) | ~1700kcal |
| Carbohydrate (g) | ~ 239 g (60%) |
| Protein (g) | ~ 48 g (11%) |
| Fat (g) | ~ 40 g (29%) |
3. Lifestyle Evaluation
Identify factors such as sedentary behaviour, irregular sleep patterns, or smoking habits that may impact diabetes management.
Lifestyle details of donors
| Lifestyle details | Donor 1 | Donor 2 | Donor 3 | Donor 4 |
|---|---|---|---|---|
| Activity level | Sedentary | Moderate | Moderate | Sedentary |
| Sleep | 7 hours | 6.5 hours | 6-7 hours | 7 hours |
| Social habits | Nil | Smoker | Nil | Nil |
Sedentary Lifestyle
A sedentary lifestyle involves minimal physical activity, often linked to prolonged sitting or inactivity. This can lead to various health issues, such as weight gain, insulin resistance, and increased risk of cardiovascular diseases, which are critical factors to consider in pre-transplant evaluations.
Irregular Sleep Patterns
Irregular sleep can disrupt the body’s circadian rhythm, leading to hormonal imbalances, stress, fatigue, and impaired glucose metabolism. This can negatively impact HbA1c levels and overall health, making it important for pre-transplant donors to adopt regular sleep schedules.
Smoking Habits
Smoking is a significant risk factor for various health conditions, including cardiovascular diseases, lung diseases, and impaired wound healing. For pre-transplant donors, smoking cessation is crucial as it can improve overall health and reduce risks during and after the transplant process. In general, lifestyle modifications, such as incorporating regular physical activity, maintaining a consistent sleep schedule, and quitting smoking, are highly recommended for pre-transplant donors to optimize their health and ensure better transplant outcomes.
2. Nutritional Intervention
A Customized Diet Plan is a tailored nutritional strategy designed to meet the specific health needs, medical conditions, preferences, and lifestyle of an individual. It involves the following key aspects:
Dietary guidelines
- Maintain portion control and follow the plate method: start with vegetables (50%), then include protein sources (25%), and finally add carbohydrates such as rice, millets, or wheat (25%)
- Avoid any form of sugar such as honey, jaggery, white sugar, sweets, pastries, cakes, chocolates and ice creams
- Include healthy fat such as avocados, nuts like almonds and walnut, seeds like sesame seeds, watermelon seeds and pumpkin seeds and fish as per dietitian recommendation.
- Include probiotics curd, skimmed paneer, buttermilk, yogurt to improve gut health.
- Limit high-calorie foods such as roots like potato, sweet potato, tapioca, fruit juices, and large bananas.
- At least five servings of diabetic friendly fruits and vegetables should be included in the diet to meet the requirements for micronutrients, antioxidants, and fibre
- Include fibre-rich sources such as millets, whole grains, raw salads, fruits, green leafy vegetables, and sprouted pulses regularly.
- Animal foods, such as processed and frozen meat that contain high amounts of saturated fat and preservatives, should be avoided. Instead, eggs, lean meat, chicken, and fish can be consumed as recommended.
- Boiling, steaming, grilling and baking without fat are preferable methods of cooking.
- Avoid trans-fat, hydrogenated fat such as fried snacks, packaged snacks and bakery items.
- Foods that provide empty calories, such as carbonated beverages, high-energy syrups, alcohol, beer, and sugary products, should be completely avoided
- Include fluids of more than 2.5 litres per day to support proper digestion and prevent constipation.
- Increase active time to more than 150 minutes per week, as per physician’s advice.
Diet recommendations
- Energy: 25–30 kcal/ kg IBW
- Carbohydrates: 50–55 % of total calories
- Protein: 15–20 % of total calories
- Fat: 25–30% of total calories
- Fibre: > 35 g/day
- Fluids: > 2.5 litres /day
Diabetic Diet plan model
| Meal timings | Menu | Quantity |
|---|---|---|
| Early Morning (6-7 am) | Detox drink (Soaked methi, Jeera, cinnamon, chia seeds, Ajwain (Omam) seeds water)/ Amla juice + Soaked Almonds 8-10nos | 200ml |
| Breakfast (8-9 am) | Millet Idly/ dosa/ upma/ Pongal Roasted Bengal gram chutney / Sambar / Boiled egg / sprouts salad Cucumber slices | 2 nos / ½ cup ¼ cup 1nos ¼ cup ½ cup |
| Midmorning (10.30- 11.30 am) | Guava/ papaya/Jamun/Berries/ pear/ Citrus fruits/ Apple+ pumpkin seeds/ watermelon seeds/ flax seeds/ sesame seeds | 150 g 15g |
| Lunch (1-2 pm) | Millets / Ancient rice (red rice/ brown rice/ black rice) or variety rice sambar/pulse/ nonveg gravy Greens / Gourd varieties vegetables/ Non starchy vegetables curd | ¼ cup ¼ cup ½ cup ¼ cup |
| Evening (4-5 pm) | Pulse veg chat (channa/ green gram/ sprouts with carrot cucumber)/ Makhana Masala Sundal Black tea /coffee without sugar | 1 cup ½ cup |
| Dinner (8-9 pm) | Millet Idly/ dosa/ upma/ Pongal Chapati / wheat Dosa Roasted Bengal gram chutney /sambar/pulse/ nonveg gravy Greens / Gourd varieties vegetables/ Non starchy vegetables | 2nos / ¼ cup ¼ cup ½ cup |
Diabetic Plate method
The Diabetic Plate Method is a simple and effective way to plan meals for managing diabetes. Here’s how you can structure it:
- Non-Starchy Vegetables: Begin by filling half of your plate with non-starchy vegetables. These include options like leafy greens, carrots, cucumbers, peppers, cauliflower, and cabbage. These vegetables are low in carbohydrates and rich in fibre, vitamins, and minerals, which help in controlling blood sugar levels
- Protein Sources: Next, allocate one-fourth of your plate to protein sources. Good protein choices for diabetics include egg, chicken, lean meat, dairy products, pulses and legumes. Protein helps in maintaining muscle mass and provides satiety, preventing overeating
- Carbohydrates: Finally, the remaining one-fourth of your plate should include carbohydrate sources include millets, rice, wheat. These carbohydrates provide energy but should be consumed in moderation to avoid spikes in blood sugar levels
This method ensures a balanced meal that supports blood sugar control and overall health. Additionally, it is important to monitor portion sizes and avoid excess salt, fruit juices, and carbonated beverages for better diabetes management
3. Monitoring and Adjustments
Daily Monitoring
- Encourage patients to maintain the meal log, activity log and sleep log
- Share a daily meal log or plate pictures to analyse nutrient intake and portion sizes.
- Update the activity log in the Kauvery health konnect app daily to track progress and motivate improvement.
Regular Monitoring
- Weekly monitoring of blood sugar levels (Fasting and Postprandial) to track progress
- Assess weight and overall nutritional status weekly once
Donors plate pictures
4. Lifestyle Modifications
Sleep Duration (>7 Hours daily)
Importance
- Adequate sleep helps regulate blood glucose levels, improve insulin sensitivity, and support overall metabolic health.
- It reduces stress hormones like cortisol, which can negatively impact diabetes management.
Implementation
- Maintain a consistent sleep schedule by going to bed and waking up at the same time daily.
- Create a conducive sleep environment by reducing noise and light disturbances and avoiding screens before bedtime.
Active Time (>150 Minutes per Week)
Importance
- Regular physical activity enhances insulin sensitivity, improves cardiovascular health, and aids in weight management.
- It also helps reduce the risk of post-transplant complications.
Implementation
- Engage in moderate aerobic activities like brisk walking, cycling, or swimming.
- Break down the weekly target into manageable sessions, such as 30 minutes for five days a week.
Post-Meal Walking
Importance
- Walking after meals helps lower postprandial blood glucose levels by improving glucose uptake in muscles.
- It reduces the risk of blood sugar spikes and aids in digestion.
Implementation
- Take a light walk for 10-15 minutes after each meal, ensuring it is not strenuous.
- Incorporate this habit as part of daily routine, gradually increasing duration if feasible.
Relaxation Techniques Before Sleep
Importance
- Relaxation techniques like deep breathing, meditation, or progressive muscle relaxation help reduce stress and promote better sleep quality.
- They lower cortisol levels, which can otherwise interfere with blood sugar regulation.
Implementation
- Practice relaxation techniques for 10-15 minutes before bedtime in a quiet and comfortable space.
- Explore guided meditations or calming music to enhance the effect.
5. Education and Counselling
- Counselled the donor, the importance of reducing sugar before the transplant.
- Advise them to adhere the suggestions for the sake of the recipient and for their own benefit to prevent post-transplant complications
- Materials provided for lifestyle modifications like sleep hygiene, warm up and cool down exercises and relaxation technique
- Provided counselling to address stress and anxiety related to the transplant process.
- Encourage them to feel positive and comfortable in following the suggestions, and provided support throughout their journey
6. Pre-Transplant Clearance
After the intervention period, the nephrologist and dietitian will re-evaluate the donor’s health status, ensuring optimal blood sugar control and overall readiness for the transplant.
Overall Benefits for Pre-Transplant Donors
- These lifestyle changes collectively improve metabolic health, stabilize blood glucose levels, and prepare the donor for surgery.
- They also promote mental well-being, reduce stress, and enhance recovery potential post-transplant.
By adopting these habits consistently, pre-transplant donors can significantly improve their readiness for the procedure and overall health outcomes.
Results
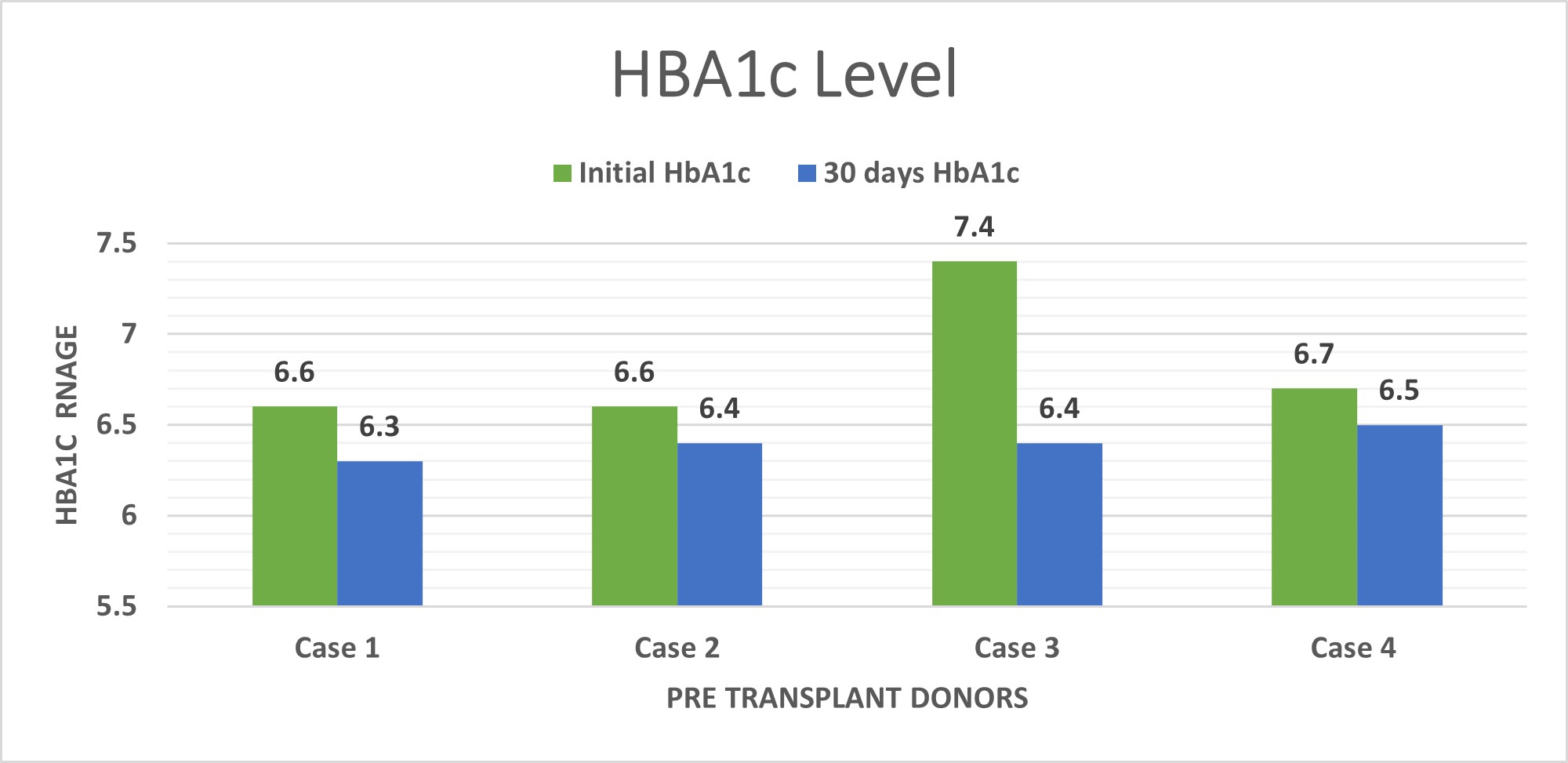
1. HbA1c
Over a period of 30 days, there has been a significant reduction in HbA1C levels, indicating improved glycaemic control. The reduction from 6.825 to 6.4 reflects effective management strategies, potentially including lifestyle changes, diet modifications, and adherence to prescribed medications or interventions. This progress is promising for diabetes management and may help in achieving long-term blood sugar control goals.
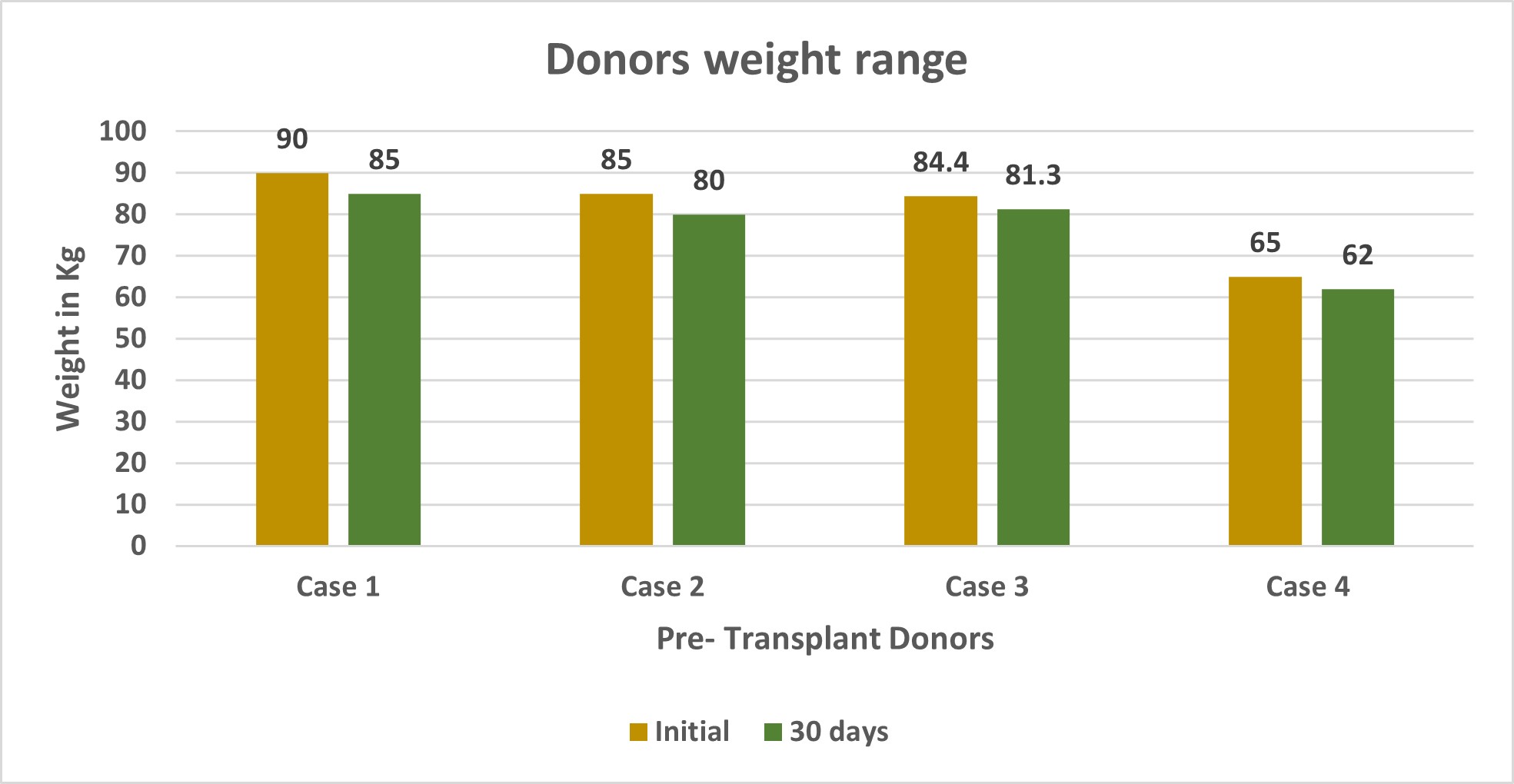
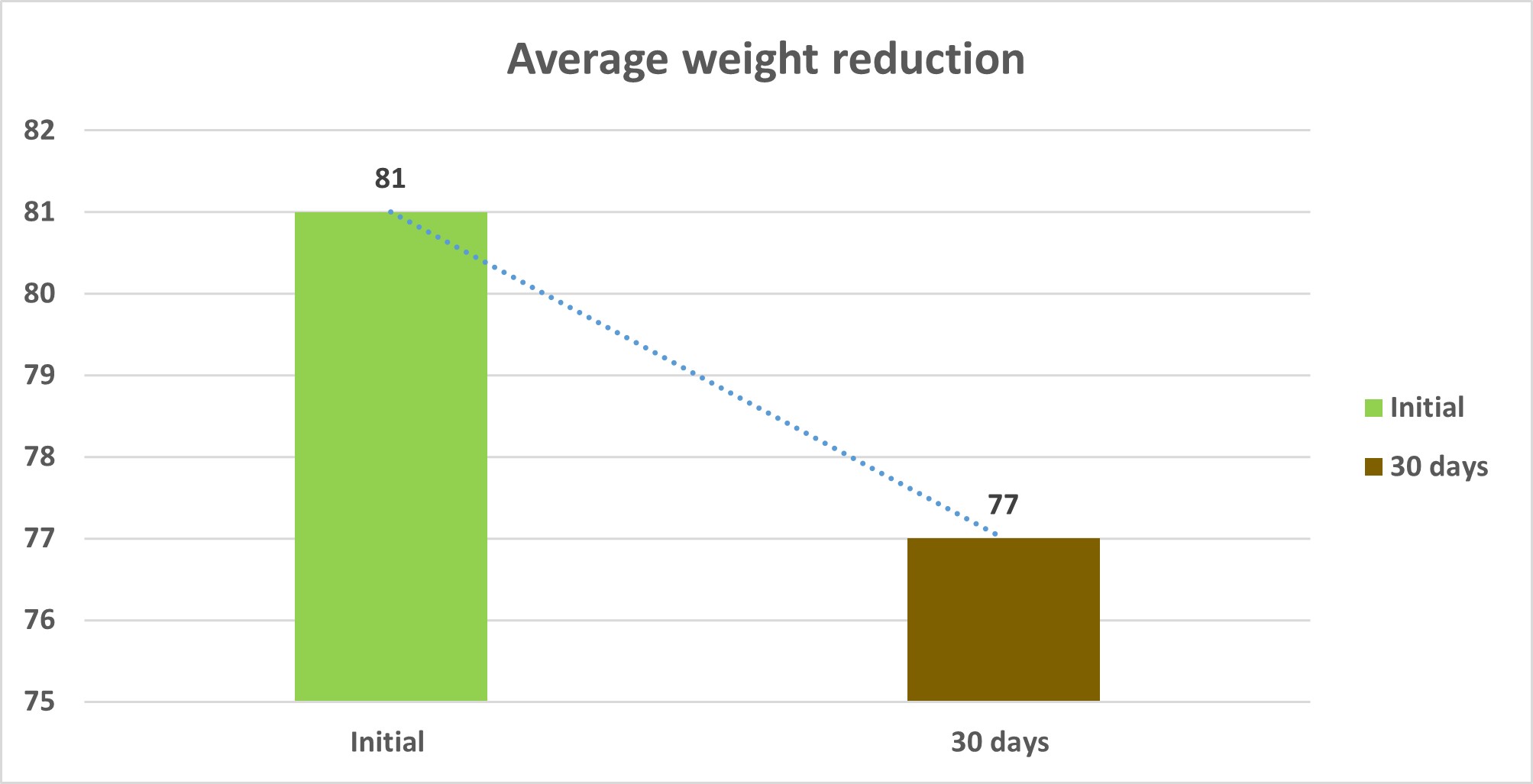
2. Weight
Over the course of 30 days, there has been a weight reduction of 4 kg, indicating effective weight management strategies. This progress may be attributed to changes in diet, increased physical activity, or adherence to a structured weight loss program. Such a reduction can contribute positively to overall health, including improved metabolic function, reduced risk of chronic diseases, and better management of conditions like diabetes or hypertension.
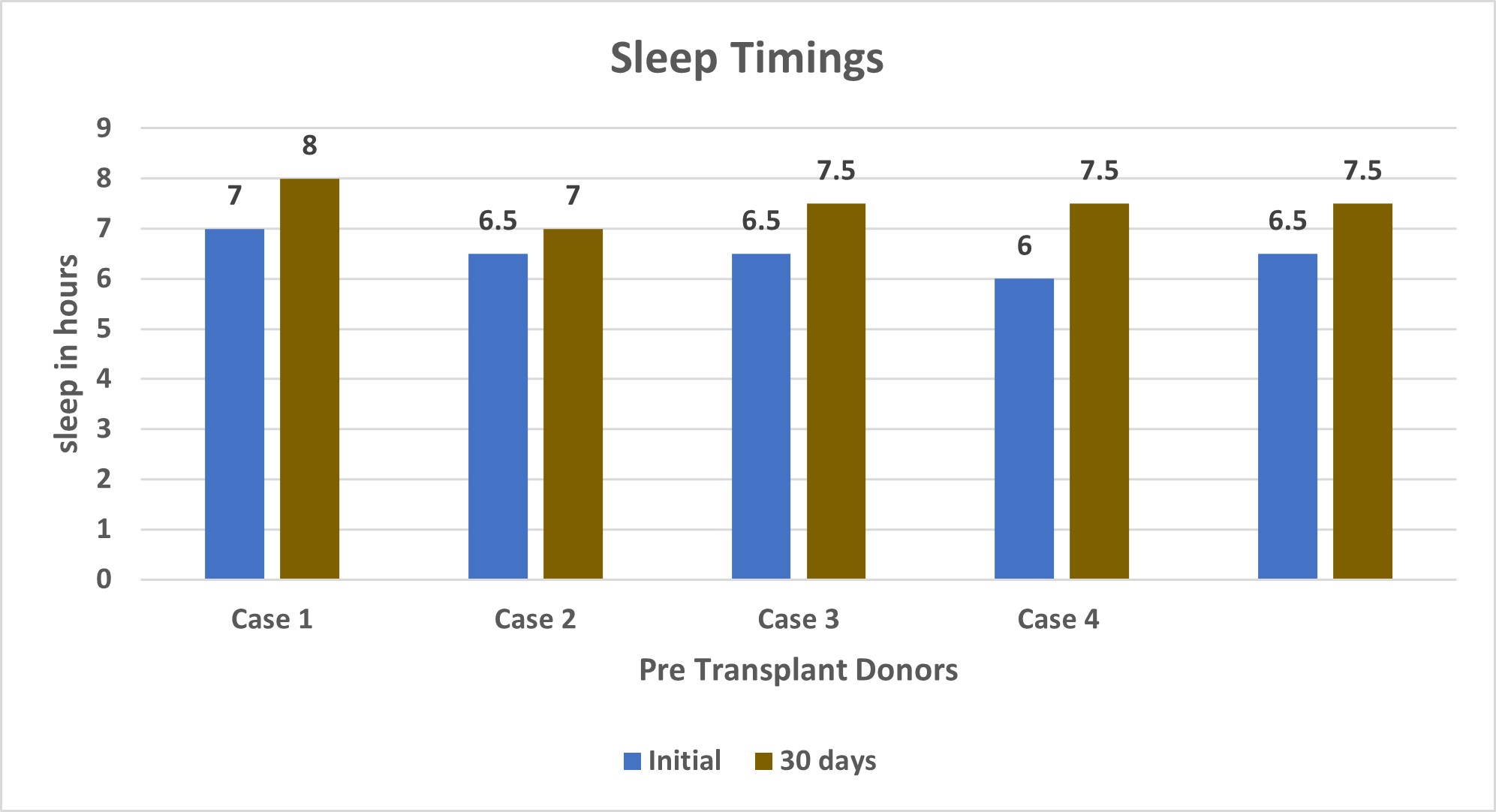
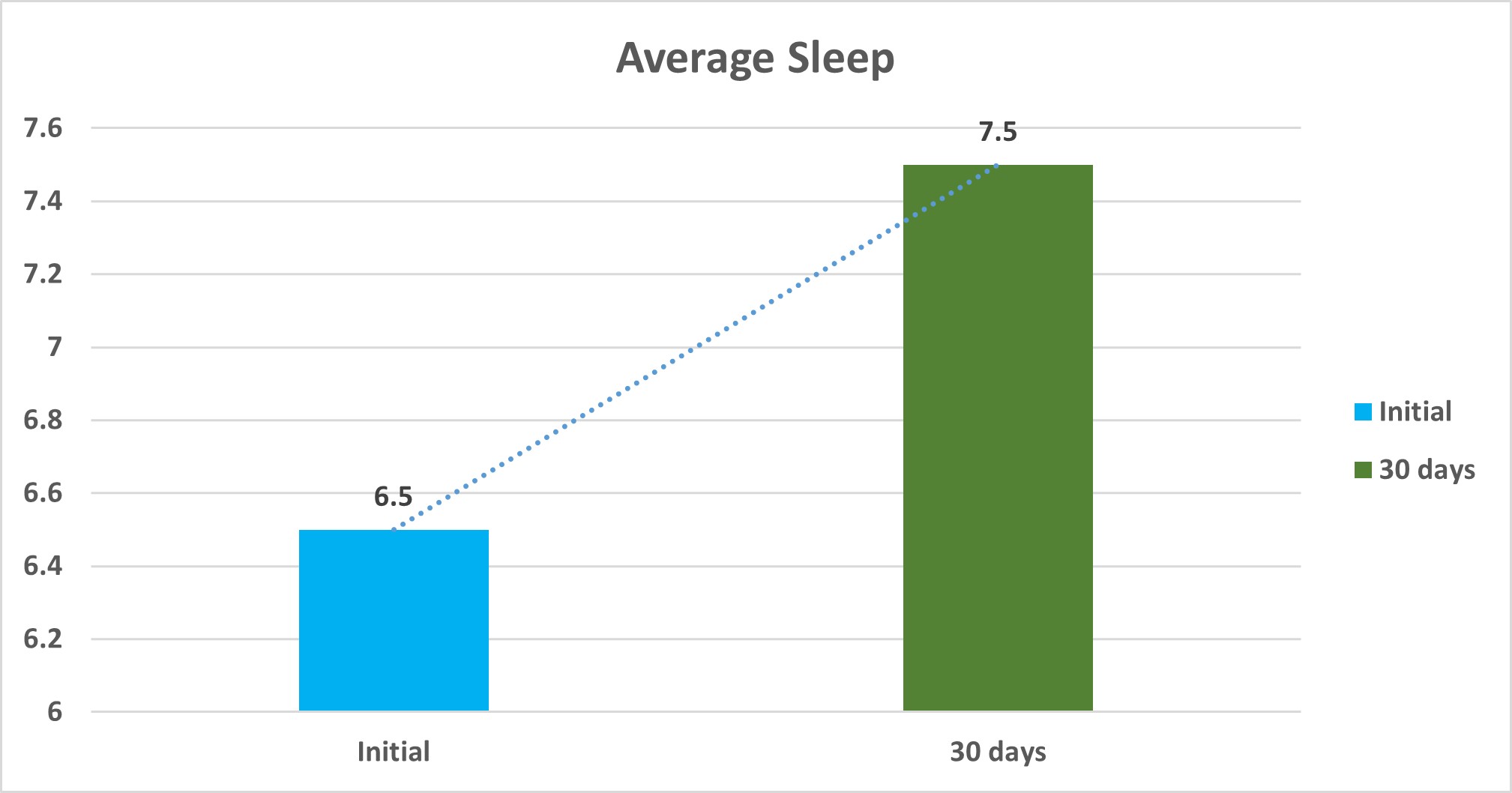
3. Sleep
Over the 30-day period, there has been a noticeable improvement in average sleep duration, increasing by 1.5 hours. This indicates better sleep hygiene or lifestyle modifications that promote longer and potentially higher-quality sleep. Improved sleep can enhance overall well-being, including better cognitive function, mood stabilization, and physical health. It may also support better management of chronic conditions and stress levels.
4. Active time
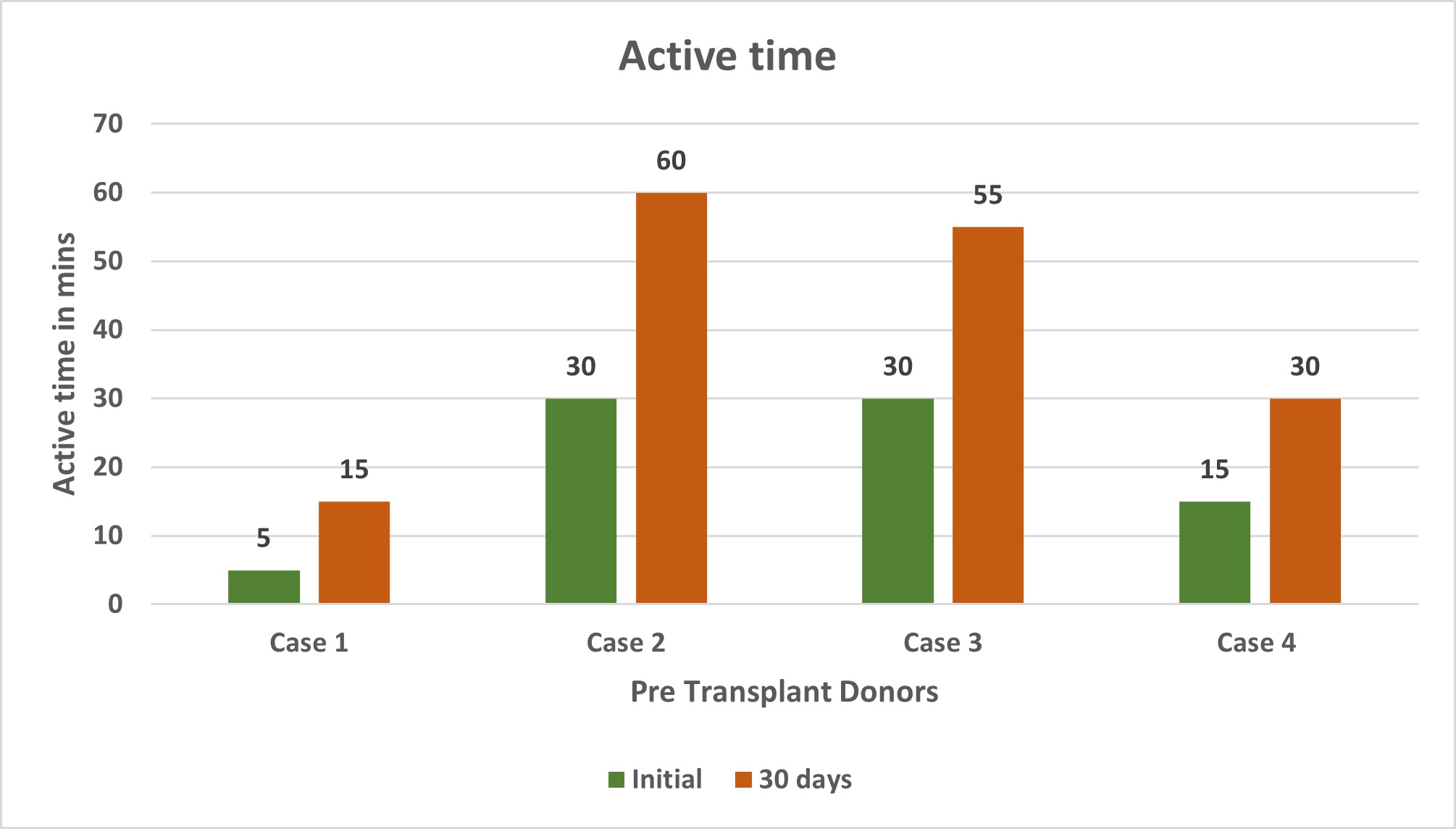
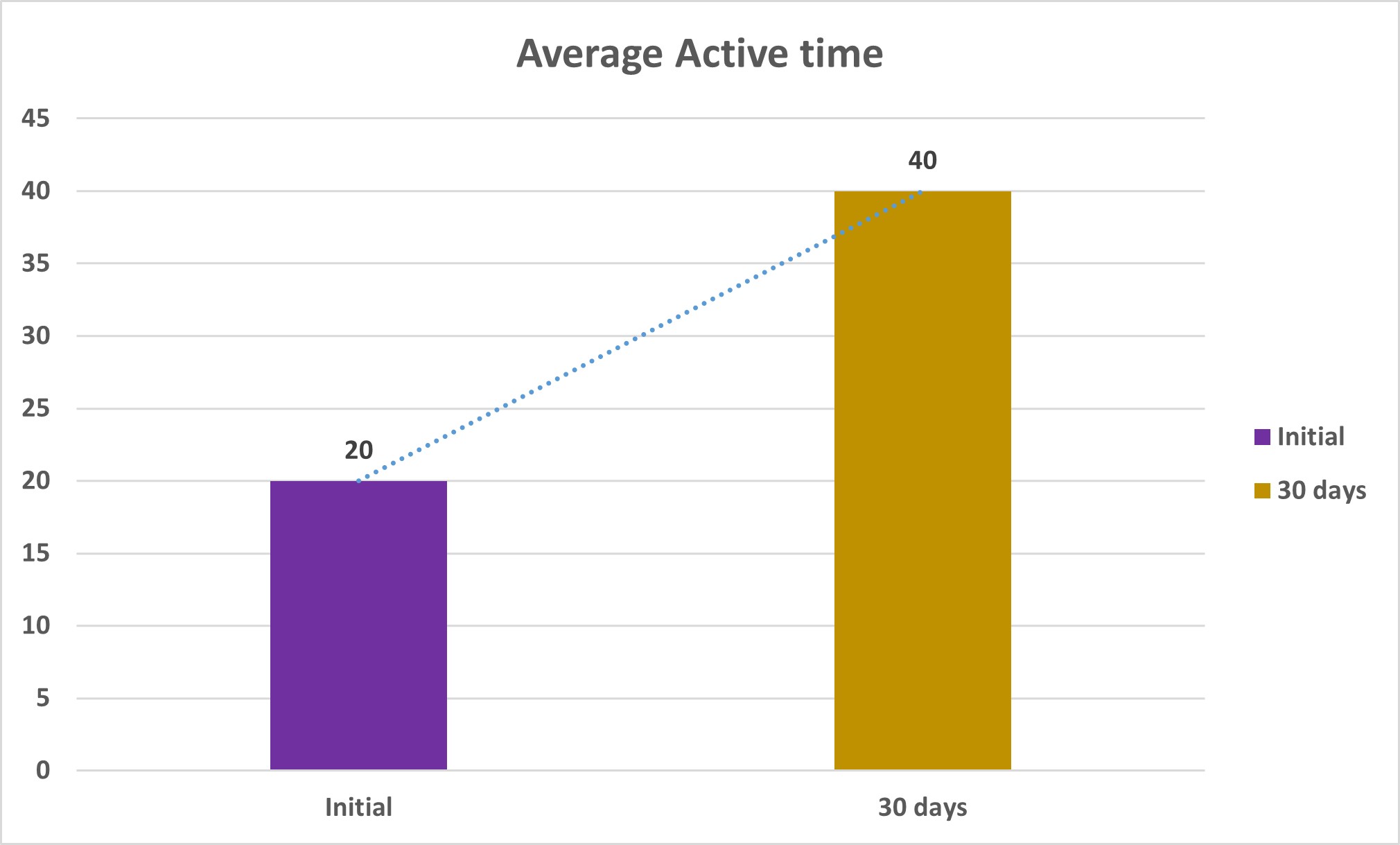
Over a 30-day period, the average active time has increased significantly by 20 minutes. This indicates improved physical activity levels, which may be the result of adopting a more active lifestyle or engaging in structured exercise routines. Increased active time contributes to better cardiovascular health, enhanced stamina, weight management, and overall physical and mental well-being. This progress reflects a positive commitment to health and fitness goals.
Conclusion
In conclusion, nutritional intervention and monitoring play a pivotal role in the effective management of diabetes. Through dietary education, personalized meal planning, lifestyle modifications, and consistent monitoring, patients are empowered to manage their blood glucose levels and improve overall health outcomes. Nutritional assessment ensures dietary plans are tailored to individual needs, while regular follow-ups provide ongoing support, motivation, and adjustments to achieve sustainable health goals. This comprehensive approach fosters better adherence, reduces complications, and enhances the quality of life for diabetic patients. In the context of shortage of compatible renal donors, our team identified four initially non eligible donors and successfully converted them into suitable candidates through targeted diet and lifestyle interventions, along with continuous clinical monitoring. Using this approach, Kauvery Hospital, Hosur, achieved successful renal transplantation with a 10% donor conversion rate, demonstrating the potential of structured modification programs to expand the donor pool and improve transplant outcomes. We conducted follow-ups with donors who had completed one year since their initial intervention. Through consistent monitoring and guidance, these donors were able to successfully maintain stable sugar levels and achieve optimal weight. This outcome was made possible by emphasizing diet and lifestyle management, Additionally, the donors were educated on the importance of balanced nutrition and the role of healthy lifestyle practices in sustaining their overall well-being. This approach not only ensured their long-term health but also demonstrated the effectiveness of a structured care plan in supporting donors’ post-intervention.
References
[1] Kidney International – “A potential living kidney donor with prediabetes” The renal consult. Volume 76, Issue 6, P673-677, September 02, 2009
[2] Delmonica,F A Report of the Amsterdam Forum on the Care of the live Kidney Donor: Data and medical Guidelines Transplantation.2005; 79: S53-S66