Penetrating stab injury to the neck (Zone II) with left subclavian artery injury and massive haemothorax
Shiva Rudrai J1, RN Gowdham P2, Vishalakshi B3
1Staff nurse – ER, Kauvery Hospital, Marathahalli, Karnataka
2Senior. Nurse Educator, Kauvery Hospital, Marathahalli, Karnataka
3CNO, Kauvery Hospital, Marathahalli, Karnataka
Abstract
Penetrating neck injuries constitute a surgical emergency due to the dense concentration of vital vascular, aerodigestive, and neurological structures. Zone II injuries pose significant diagnostic and therapeutic challenges. We report the case of a 21-year-old male who presented in haemorrhagic shock following a penetrating stab injury to the left side of the neck. Initial external wound suturing at a peripheral facility masked the severity of the underlying vascular injury. Contrast-enhanced computed tomography angiography revealed dual lacerations of the left subclavian artery with associated pleural rent and massive haemothorax. The patient underwent emergency combined supraclavicular neck exploration and left thoracotomy with successful vascular repair. This case highlights the importance of structured trauma assessment, early imaging, multidisciplinary coordination, and vigilant nursing care in improving outcomes following life-threatening penetrating neck trauma.
Keywords: Penetrating neck injury; Zone II; Subclavian artery injury; Haemothorax; CT angiography; Trauma nursing
Introduction
Penetrating neck injuries account for a small but significant proportion of trauma-related emergencies and are associated with high morbidity and mortality due to the compact anatomy of the cervical region. The neck is traditionally divided into three anatomical zones to guide evaluation and management. Zone II, extending from the cricoid cartilage to the angle of the mandible, contains major vascular structures, the aerodigestive tract, and multiple cranial nerves. Although modern trauma algorithms increasingly favor selective, imaging-guided management in hemodynamically stable patients, the presence of hard signs of vascular injury necessitates immediate surgical exploration. This case report describes a complex Zone II penetrating neck injury complicated by left subclavian artery laceration and massive hemothorax, emphasizing the critical role of timely diagnosis, surgical intervention, and comprehensive nursing care.
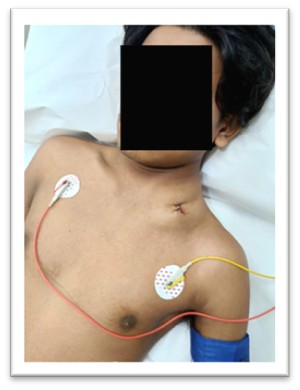
A 21-year-old male was referred to the Emergency Department following an alleged assault resulting in a stab injury to the left side of the neck. He had initially presented to a nearby healthcare facility, where first aid was administered and the external wound was sutured. Due to progressive clinical deterioration, he was transferred to our hospital for advanced management.
Clinical Presentation on Arrival
On arrival, the patient was breathless, hypotensive, drowsy, and showed clinical features consistent with Class III–IV haemorrhagic shock. In accordance with Advanced Trauma Life Support (ATLS) principles, priorities included airway assessment, evaluation of breathing, and circulatory stabilization. Given the alleged assault, the case was registered as a Medico-Legal Case (MLC) following initial resuscitation, as per institutional protocol.
Examination Findings
Primary Survey (ABCDE)
- Airway (A): Patent; patient able to speak; no stridor, haemoptysis, or overt airway obstruction.
- Breathing (B): SpO₂ 94% on room air; reduced air entry on the left hemithorax; suspicion of haemothorax/pneumothorax.
- Circulation (C): Pulse 110/min; blood pressure 80/50 mmHg (permissive hypotension); capillary refill time >3 seconds; cold peripheries; no active external bleeding; weak but palpable left brachial, radial, and ulnar pulses; no carotid thrill.
- Disability (D): Glasgow Coma Scale 14/15; lethargic but oriented; pupils equal and reactive; moving all four limbs.
- Exposure (E): Large expanding hematoma over the left neck extending to the clavicle and midline; a 1 × 2 cm sutured penetrating wound over Zone II; no other external injuries identified.
Local Examination
A significant hematoma was noted over the left supraclavicular region and posterior triangle, extending from the clavicle to the angle of the mandible. Diminished left upper limb pulses raised concern for vascular compromise, and the clinical picture suggested a possible pleural and thoracic outlet injury.
Emergency Department Management
Initial Resuscitation
The patient was managed as haemorrhagic shock with cautious permissive hypotension. Two large-bore intravenous cannulas were secured, intravenous crystalloids were initiated, and one unit of O-positive packed red blood cells was transfused. Tranexamic acid was administered to reduce ongoing haemorrhage. Supportive care included analgesics, antiemetics, tetanus prophylaxis, and broad-spectrum intravenous antibiotics.
Investigations
- Laboratory: Complete blood count, renal and liver function tests, coagulation profile, blood grouping, and crossmatching were performed. Arterial blood gas analysis revealed haemoglobin of 9.6 g/dL.
- Imaging: Chest X-ray demonstrated a left-sided haemothorax. Contrast-enhanced CT angiography of the neck and chest was performed for definitive assessment.
CT Angiography Findings
CT angiography revealed a large hematoma along the trajectory of the penetrating injury, compressing structures at the thoracic outlet. Two lacerated rents were identified in the left subclavian artery one anterior-superior and another posterior. The hematoma extended into the mediastinum, with proximity to the left phrenic nerve. A massive left-sided haemothorax with associated pneumothorax and an apical pleural rent was also noted. These findings mandated emergent surgical intervention.
Surgical Management and Intensive Care
Given the presence of multiple hard signs of vascular injury including haemorrhagic shock, expanding hematoma, diminished distal pulses, and CT-confirmed subclavian artery laceration the Cardiothoracic and Vascular Surgery (CTVS) team was urgently involved. After rapid multidisciplinary discussion, the patient underwent emergency surgery under general anaesthesia.
A combined supraclavicular neck exploration and left thoracotomy was performed. The supraclavicular incision incorporated the stab wound, and the hematoma along the penetrating tract was carefully evacuated. Proximal and distal control of the left subclavian artery was achieved, and two arterial lacerations were repaired using 6-0 Prolene sutures. Avulsed arterial and venous branches were clipped. A rent in the left pleura was repaired, and a massive haemothorax was evacuated. A left intercostal drain was inserted, draining approximately 2 Liters of blood intraoperatively. The wound was closed in layers.
The patient received a total of three units of packed red blood cells intraoperatively and postoperatively. He was shifted to the Intensive Care Unit, where he remained hemodynamically stable. Close monitoring focused on airway patency, neurological status, and limb perfusion. Postoperative Doppler ultrasonography of the left upper limb demonstrated normal arterial flow with no evidence of thrombosis.
Outcome and Follow-Up
Then the patient showed significant clinical improvement. The intercostal drain was removed after confirmation of full lung expansion and minimal drainage. The patient remained hemodynamically stable with intact distal pulses and no neurological deficits. Upper limb motor strength returned to baseline. He was discharged on oral antibiotics, analgesics, proton-pump inhibitor therapy, low-dose aspirin, and psychiatric medication as advised. Follow-up was scheduled in the CTVS outpatient clinic, and detailed counselling on red-flag symptoms was provided to the patient and caregivers.
Nursing Diagnoses and Care
Key nursing diagnoses included impaired gas exchange, deficient fluid volume, acute pain, risk of infection, risk of ineffective cerebral tissue perfusion, and anxiety. Nursing care emphasized continuous airway surveillance, hemodynamic monitoring, transfusion support, chest drain care, pain management, infection prevention, neurological observation, and psychological support. Comprehensive discharge education was provided to promote recovery and early detection of complications.
Discussion
Penetrating neck injuries remain among the most complex trauma scenarios due to the high density of vital structures within a confined anatomical space. This case underscores the limitations of relying solely on external wound appearance, as initial suturing masked a life-threatening vascular injury. The presence of hard signs of vascular injury necessitated immediate surgical exploration, in keeping with established trauma guidelines. CT angiography proved invaluable in delineating the extent of vascular and thoracic injury, facilitating prompt operative planning.
Neck Injuries: Anatomical Zones, Structures, Complications & Management
| Neck Zone | Anatomical Boundaries | Major Structures at Risk | Common Complications | Preferred Management Approach |
|---|---|---|---|---|
| Zone I | Clavicle → Cricoid cartilage | Subclavian vessels, carotid artery origins, vertebral artery, trachea, oesophagus, apex of lung, thoracic duct, vagus & recurrent laryngeal nerves | Massive hemorrhage, hemothorax, pneumothorax, tracheal injury, oesophageal perforation, vertebral artery injury, airway obstruction | CT angiography; high suspicion for thoracic outlet injuries; often requires thoracotomy or sternotomy; airway protection; selective vs mandatory exploration depending on stability |
| Zone II | Cricoid cartilage → Angle of mandible | Common carotid, internal & external carotid arteries, internal jugular vein, larynx, trachea, pharynx, esophagus, vagus nerve, spinal accessory nerve | Airway compromise, expanding hematoma, stroke from vascular injury, aerodigestive tract injury, massive hemorrhage | Traditionally mandatory exploration; now selective management with CT angiography in stable patients; immediate surgery for unstable patients or hard signs |
| Zone III | Angle of mandible → Base of skull | Distal internal carotid artery, external carotid branches, vertebral artery, parotid gland, cranial nerves IX–XII | Carotid dissection, cranial nerve palsies, airway swelling, inaccessible vascular injuries | CT angiography; often requires endovascular intervention such as stenting or coiling due to difficult surgical exposure; selective exploration; airway protection as needed |
Signs and symptoms of neck injury
| Category | Hard Signs (Mandate Immediate Surgical Exploration) | Soft Signs (Require Further Evaluation) |
|---|---|---|
| Vascular Injury |
|
|
| Laryngotracheal Injury |
|
|
| Pharyngoesophageal Injury | — |
|
From a nursing perspective, vigilant monitoring, early recognition of deterioration, and coordinated perioperative care were critical in optimizing outcomes. Multidisciplinary collaboration among emergency medicine, anaesthesia, cardiothoracic and vascular surgery, radiology, critical care, and nursing teams played a decisive role in patient survival and recovery.
Nursing Diagnoses
The following nursing diagnoses were identified during the patient’s acute and postoperative care:
- Ineffective Airway Clearance / Impaired Gas Exchange related to neck hematoma, pleural injury, and potential airway compromise secondary to penetrating neck trauma.
- Risk for Aspiration due to the possibility of oesophageal or pharyngeal involvement and altered sensorium from shock and analgesia.
- Deficient Fluid Volume associated with major vascular injury, haemorrhagic shock, and ongoing blood loss.
- Acute Pain related to soft tissue trauma, vascular injury, pleural rent, and surgical interventions.
- Risk for Infection due to penetrating wound, foreign material exposure, and risk of contamination from aerodigestive structures.
- Risk for Ineffective Cerebral Tissue Perfusion associated with compromised subclavian artery flow and risk of cerebrovascular ischemia.
- Anxiety and Fear related to the traumatic nature of the injury, emergency interventions, and uncertainty regarding prognosis and surgical outcomes.
- Nursing care focused on continuous airway surveillance, hemodynamic monitoring, pain management, infection prevention, psychological support, and early identification of complications.
Conclusion
This case highlights the critical importance of structured trauma assessment, early imaging, and timely multidisciplinary intervention in managing penetrating Zone II neck injuries. Prompt recognition of vascular injury and emergent surgical repair of the left subclavian artery were lifesaving. Comprehensive nursing care and patient education further contributed to a favourable outcome. Early detection, decisive action, and coordinated teamwork remain essential to reducing morbidity and mortality in penetrating neck trauma.