Exclusion of infra renal abdominal aneurysm with aorta bi-iliac bypass
Pushpa1*, Anitha2
1OT Nursing Incharge, Kauvery Heart City, Trichy, Tamil Nadu
2OT Senior Staff Nurse, Kauvery Heart City, Trichy, Tamil Nadu
*Correspondence
Abstract
An abdominal aortic aneurysm (AAA) is often asymptomatic, detected incidentally, but symptoms can include a pulsatile feeling near the belly button, and deep pain in the abdomen or back. A ruptured AAA is life-threatening, presenting severe, sudden back or abdominal pain, and signs of shock including low blood pressure. A palpable pulsatile mass in the abdomen is also a key sign, though not always present.
Background on AAAs
An abdominal aortic aneurysm (AAA) is defined as a permanent dilation of the abdominal aorta, with a diameter greater than 3 cm or a diameter greater than 50% of the aortic diameter at the level of the diaphragm. If left untreated, progressive vessel wall degeneration leads to dilation and thinning of the vessel. Eventually, these changes can result in the rupture of the AAA. AAA prevalence and incidence rates have decreased over the last 20 years, both in developed and in developing countries. This decrease has been attributed partially to the decline in smoking. Prevalence is negligible before the age of 55 to 60 years, and after that, the prevalence increases with age. AAA prevalence is up to fourfold more in men (between 1.3% and 12.5%) than women (between 0.0% and 5.2%). The risk of rupture increases with the size of the aneurysm: the 5-year risk for aneurysms less than 5 cm is 1% to 2%, whereas it is 20% to 40% for aneurysms greater than 5 cm in diameter. Abdominal aortic aneurysm represents about 1% of deaths in males over the age of 65 and is the tenth leading cause of death in men 65 years of age or older. The mortality rate of ruptured abdominal aortic aneurysm is over 80%. Early diagnosis and treatment, therefore, are very important before its rupture.
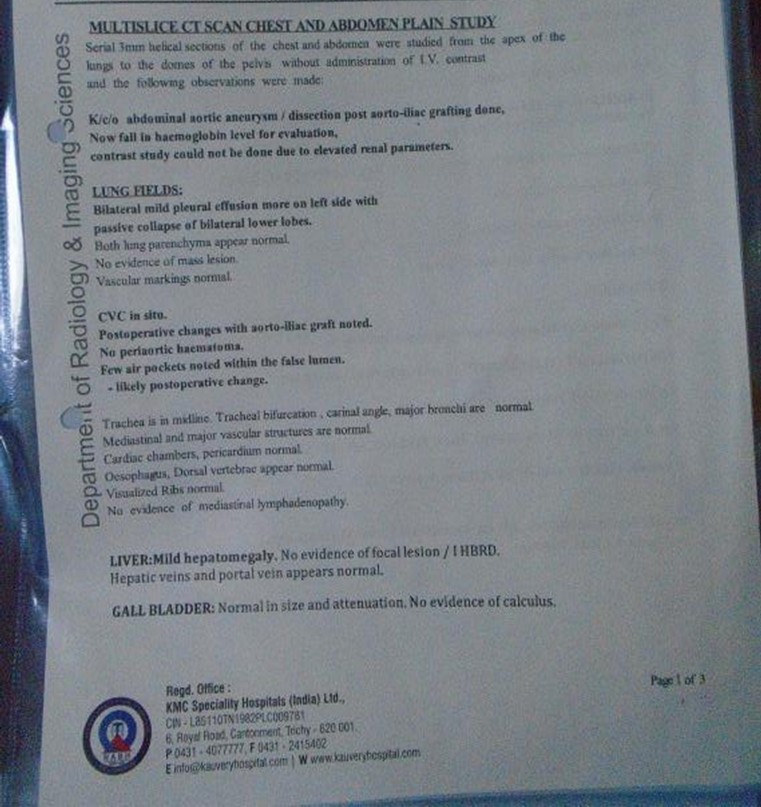
A 39 years old Female, known case of hypothyroidism for 10 years, complaints of sudden onset of pain abdomen since 04/11/2025and was evaluated further management in outside hospital, during her admission patient had episode of vomiting and increased abdominal pain for which CT Angio have been done which showed descending thoracic aorta and abdominal aortic aneurysmal dilation with dissection with aneurysm extending into right CIA. Patient was sent home for conservative management where she developed vomiting again and went to Meenakshi hospital where initial treatment has been given and referred here for further management. On receiving, patient was conscious, oriented and her vitals were stable. CT abdomen done showed DTA aneurysm with dissection infrarenal aortic aneurysm extending up to CIA? Mycotic origin. The patient admitted and planned for staged repair of TAAA. Cardiologist opinion was obtained and his orders were carried out. patient underwent Excision of infra-renal abdominal aneurysm with Aorta Bi-Iliac bypass using 18 × 9 mm unigraft.
On examination
- Patient conscious, oriented
- BP – 120/80 mmhg
- HR – 80b/min
- SpO2 – 99% at RA
- RR – 11/min
- Temp – Normal
- CVS – S1 S2+
- RS – B/L AE+
- P/A – Soft
- CNS – NFND
- HT – 146cms
- WT – 38kgs
Pre OP Medication
- Tamin 1G IV SOS
- Emeset 4mg IV SOS
- IV Fluids 60ml/hr on flow
Pre OP Investigation
- Hb – 10.2 g/dl
- PCV – 32.2%
- RBC Count – 4.41ML/10^9
- WBC Count – 11970 Cells/Cumm
- Platelet – 396000Cells/Cumm
- GCT – 102mg/dl
- Urea – 29.96mg/dl
- Creatinine – 0.91mg/dl
- Na – 135mmol/L
- K – 3.60mmol/L
- Blood grp – B +
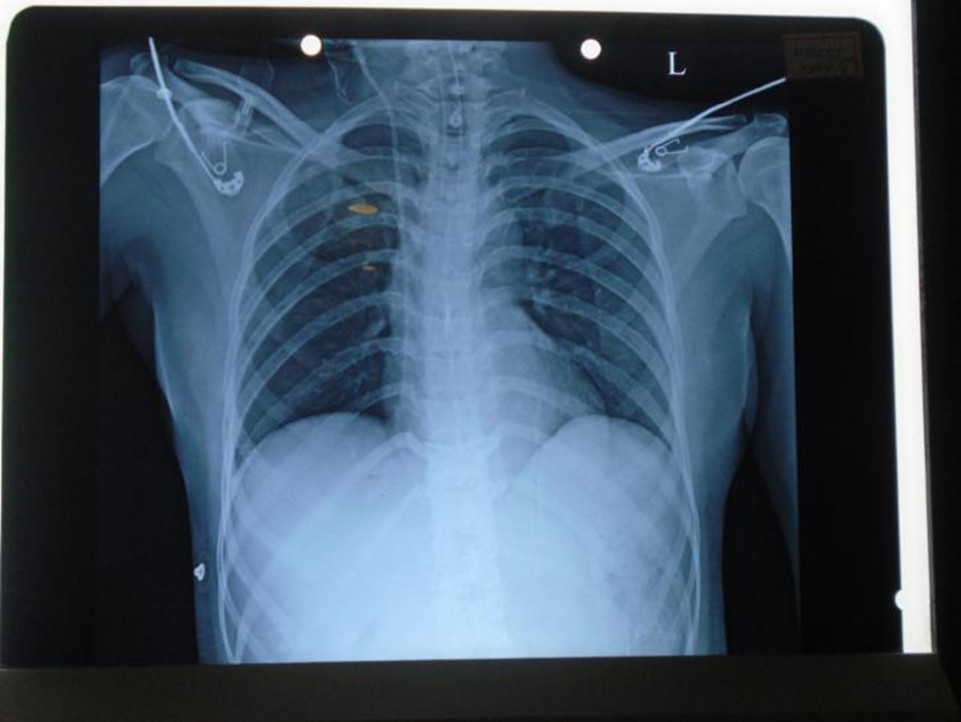
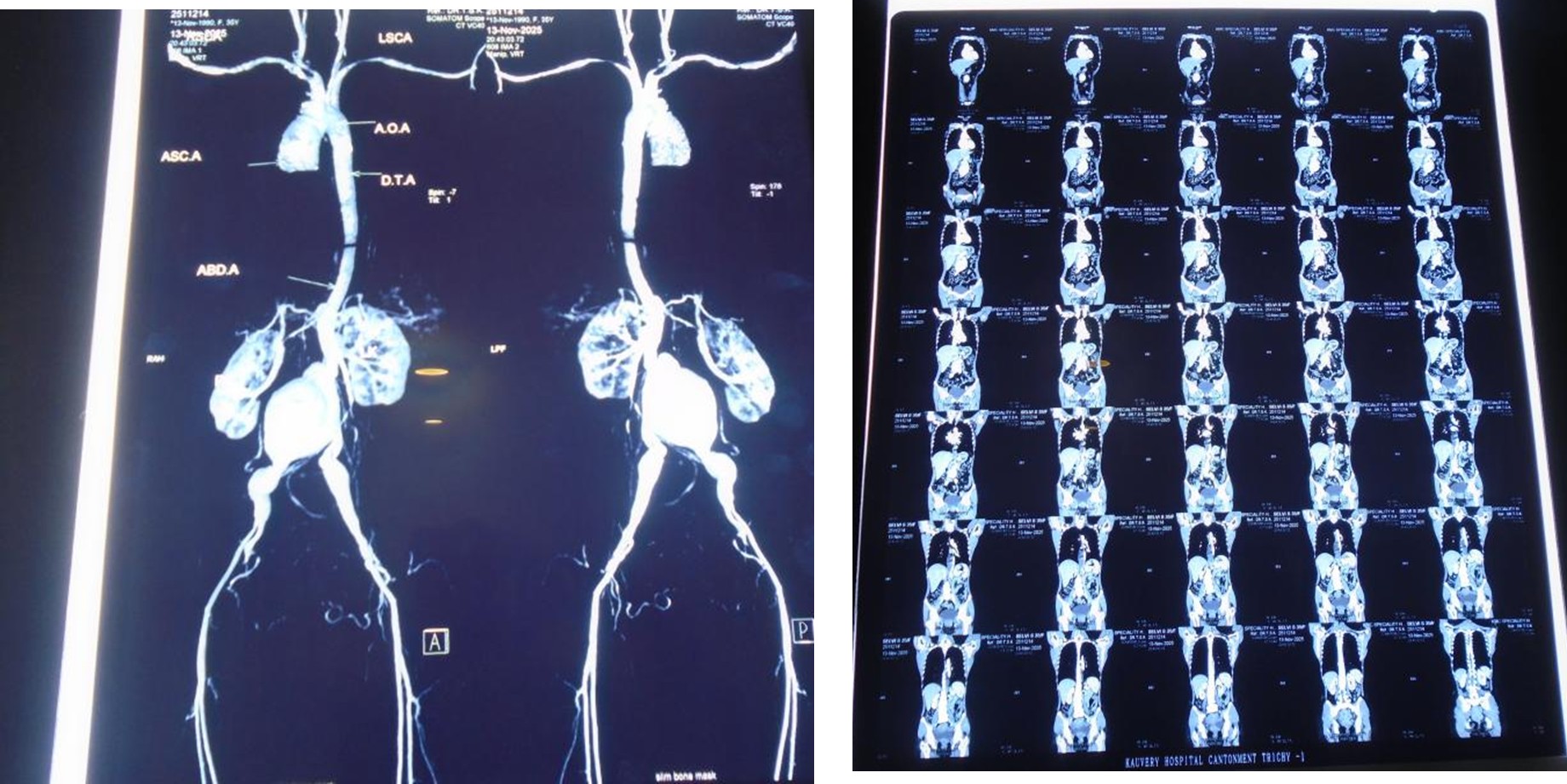
Pre OP X-Ray
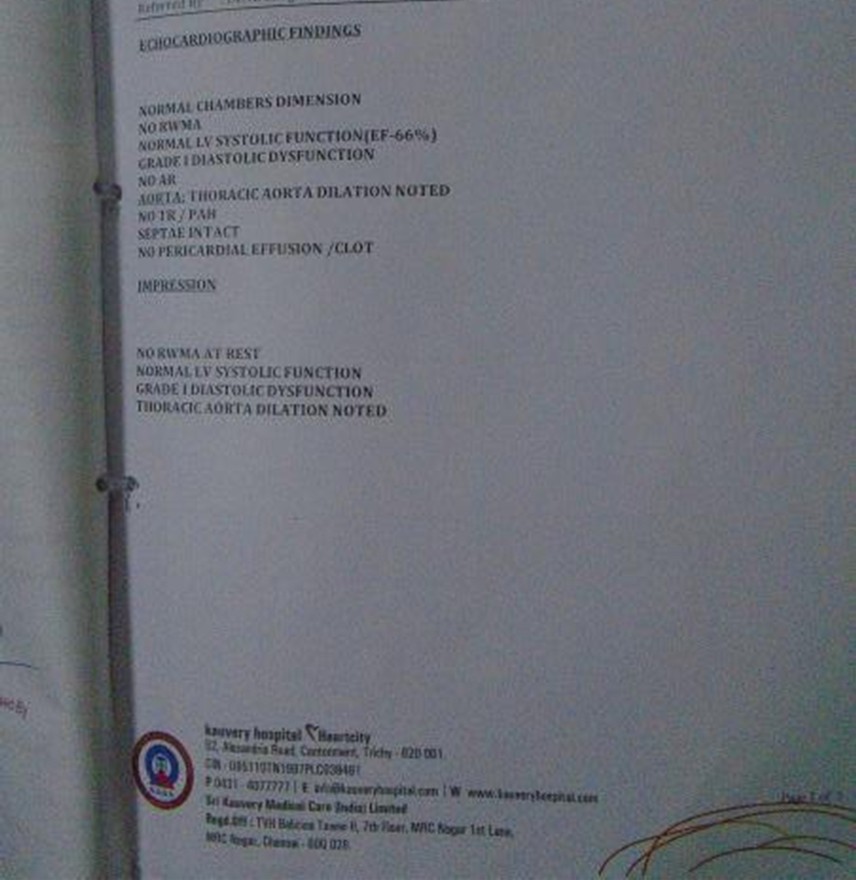
ECHO
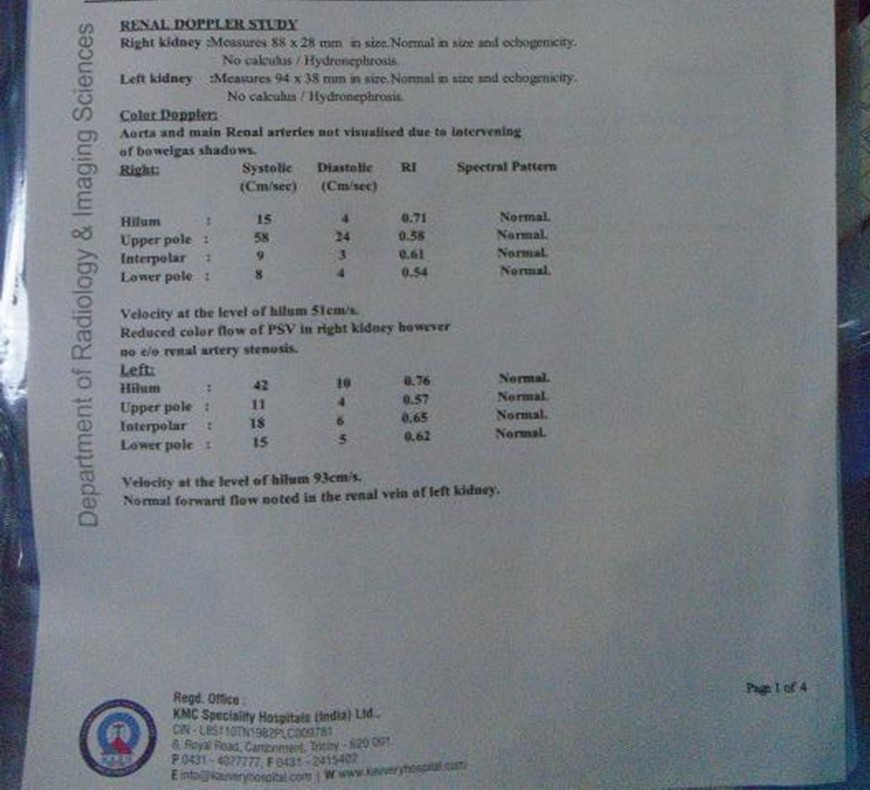
Carotid Doppler
CT Angio
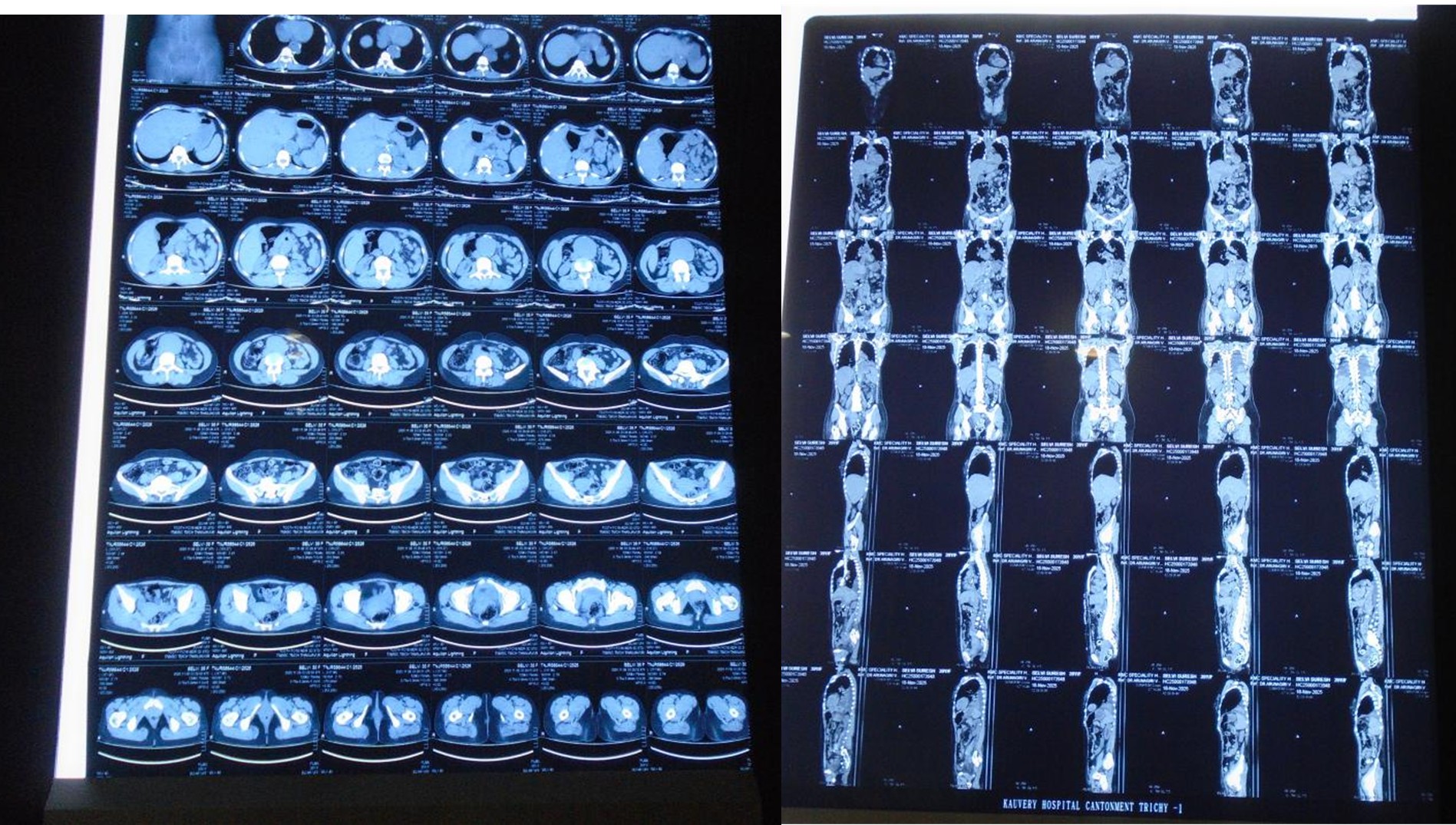
CT Scan Report
Operation Notes
Surgery: Exclusion of Infrarenal Abdominal aneurysm with Aorta BI- Iliac bypass using 18 × 9 mm uni – graft
Procedure
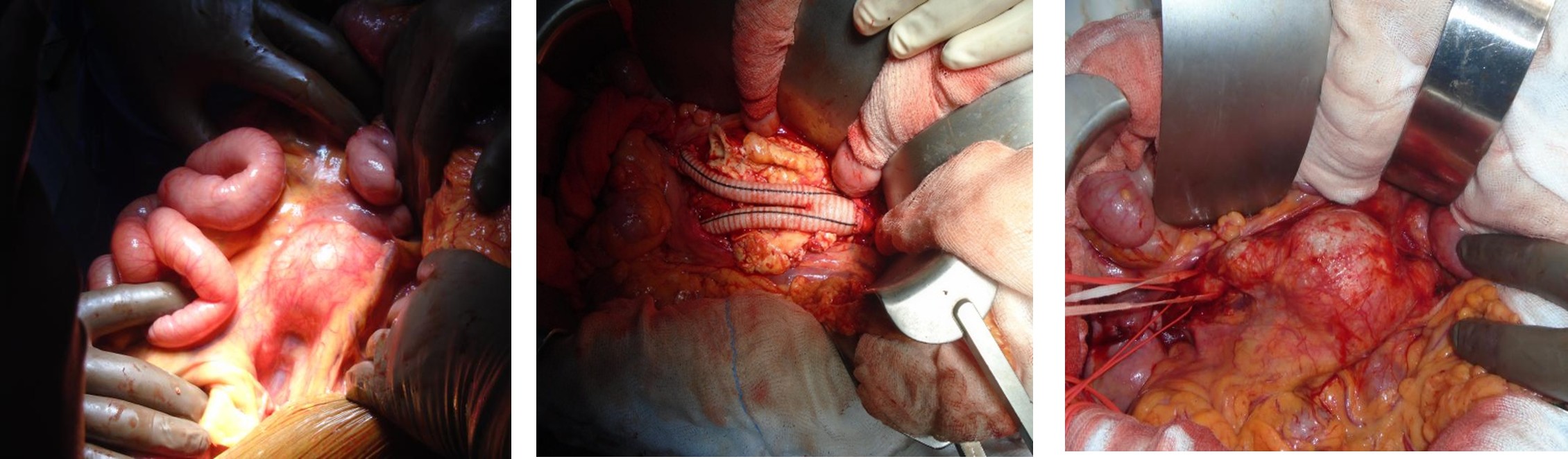
Step 1: Laparotomy
- Skin incision from Xiphi sternum to supra region given
- Rectum Opened in midline and peritoneum opened
- Small bowel /large bowel /liver checked for any malignancy.
- Aneurysm dilatation of the aorta noted. On Retracting small bowel to right side, dissection above the aneurysm done.
Step 2: Iliac Artery Control
- Dissection done near right CIA Ureter was carefully dissected and kept away.
- Right CIA/ELA/ELA control taken.
- Both the CIA were found to be Aneurysmal
Step 3: Excursion of the aneurysm Sac
- Dissection cattier above the aneurysm and left renal vein was identified.
- Left Renal vein divided and repaired the end and 6-0 prolene Kessler’ technique
- Inferior mesenteric vein was also legated
- Periaortic tissues was legated carefully
- Both the right RA and Left RA were dissected and separated
- Clamp space created between the renal arteries
- Heparin 25000U given and ACT was monitored
- ACT: After 3 minutes 246 After 10 minutes 192
- Proximal clamp over the aorta applied – inter renal clamp applied -right RA perfusing
- Distal clamp over the bilateral iliac arteries applied
- Aneurysm checked for any pulsation.
- Once no pulsation confirmed it was opened in midline
- The wall the Aneurysm sac was Excised and sent for HPE/C/D/TB Sampling
- Posterior walls that bleed from lumbar vessels were repaired using 3-0 prolene
- On Opening the aortic sac, a clear septum dividing the true and false lumens was noted. The true lumen was very small, and the false lumen was thrombosed.
- Excision of the septum was done through debridement and was given.
Step 4
- Proximal anastomosis between uni graft B-Braun 18 x 9/40cm and aorta done using 4-0prolene
- Minimal Bleeding noted from IVC – which was repaired using 5.0 prolene
- Once proximal anastomosis was over clamp was shifted distally to graft
- Graft was brought done through Retro peritoneum, bilateral distal anastomosis done using 5.0 prolene through was given and hemostasis achieved.
- Omentoplasty done.
- Rectus sheath closed with loop Ethilon.
Procedure
Benefits of Excision of Infra-renal Abdominal Aneurysm with Aorta Bi-iliac Bypass:
- Prevents life-threatening aneurysm rupture
- Restores safe blood flow to the lower body and legs
- Improves walking ability and reduces leg pain from poor circulation
- Provides long-lasting results with durable grafts
- Enhances overall quality of life and survival rate
Post OP Orders
- RT aspiration.
- IV Fluids administered as per intensivist orders.
- Magnex Forte 1.5 g IV BD
- Targocid 400mg IV BD one-day f/b OD
- Pan 40 mg IV OD
- Intake /Output vitals charting.
- Cultures and HPE sent for lab.
Post-Operative Period
- POD
- Patient received from HCOT with AMBU bag ventilation then connected with mechanical ventilator.
- Mode – SIMV(PRVC+PS)
- Fio2 -100%, PEEP- 5cmof H2O, TV-350ml
- Patient vitals were stable.
- She was managed with necessary support.
- Bupivacaine 4ml /hr.
- Noradrenaline 2.5ml/hr.
- Propofol 5ml/hr.
- Every 4h patient was given back care and ET suctioning
- Antibiotic Inj. Cefactum 1.5g IV BD administered
1st POD
- Patient vitals are stable.
- Extubation done.
- She was managed with necessary support.
- Noradrenaline 2.0ml/hr.
- Bupivacaine 4ml /hr.
- Early in the morning patient was given mouth care, combing and dressing done.
- Tapper Inotropic , anticoagulant tomorrow onwards start mobilizing and Chair sitting plan
2nd POD
- Patient vitals are stable.
- She was managed with necessary support.
- Bupivacaine 7ml /hr.
- Early morning patient was given mouth care, combing and dressing done.
- Oral Sip of Water given.
- Aterial line removed.
- Dressing Changed.
- USG Scan Advised taken.
- Steam Nebulization Given.
- Spiro & Chest Physio given.
- Back Care Given.
3rd POD
- Patient vitals are stable.
- Oral Liquid diet started.
- Chest physiotherapy given.
4TH POD
- Patient vitals are stable.
- Patient shifted to the ward with stable status.
| S No | Investigation | 0-POD | 1st - POD | 2nd - POD | 3rd- POD | 4th - POD |
|---|---|---|---|---|---|---|
| 1 | Hb | 12.4 | 12.9 | 12.7 | 6.8 | 9.1 |
| 2 | PCV | 31 | 38.6 | 34 | 20.8 | 27.0 |
| 3 | Urea | - | 53.50 | - | 66.34 | 96.30 |
| 4 | Creatinine | - | 1.98 | - | 0.97 | 2.97 |
| 5 | Na | 133 | 136 | 133 | 142 | - |
| 6 | K+ | 4.6 | 5.16 | 6.2 | 3.62 | 4.40 |
| 7 | Ph | 7.35 | 7.47 | - | - | - |
| 8 | PO2 | 556 | 206 | - | - | - |
| 9 | PCo2 | 32 | 33 | - | - | - |
| 10 | HCO3 | 19.6 | 25.6 | - | - | - |
| 11 | Glucose | 238 | 153 | - | - | - |
Nursing Diagnosis
Preoperative Nursing Diagnose
- Anxietyrelated to the potential complications of surgery and the threat to health status.
- Fearrelated to the surgical procedure and potential outcomes.
- Deficient knowledgerelated to the condition, surgical procedure, and necessary postoperative care/lifestyle modifications.
Postoperative Nursing Diagnoses
- Acute Painrelated to surgical tissue trauma and the presence of an abdominal incision.
- Risk for Decreased Cardiac Outputrelated to potential changes in intravascular volume, third-space fluid shift, or increased systemic vascular resistance.
- Ineffective Breathing Patternrelated to the effects of general anesthesia, endotracheal intubation, and abdominal incision.
- Risk for Bleeding(Hemorrhage) related to the surgical site and the nature of vascular surgery.
- Risk for Infectionrelated to the surgical incision, presence of invasive lines (e.g., urinary catheter, IV lines, arterial lines), and a potential for ischemic bowel.
- Risk for Ineffective Renal Perfusionrelated to the potential effects of aortic cross-clamping during surgery.
- Risk for Ineffective Peripheral Tissue Perfusionrelated to potential graft complications or embolization.
- Risk for Impaired Physical Mobilityrelated to activity restrictions and the recovery process.
- Risk for Constipationrelated to immobility, anesthesia effects, and pain medication.
- Risk for Ineffective Sexuality Patterns (Male)related to possible impotence or loss of ejaculation because of nerve damage during surgery.
- Readiness for Enhanced Self-Health Managementas the patient transitions to home care with activity restrictions and the need for lifestyle changes (e.g., smoking cessation, diet, exercise).
Pre-operative Nursing Management
The primary goal is to optimize the patient’s condition for surgery and prevent aneurysm rupture.
Assessment
- Monitor vital signs closely, especially blood pressure (BP), as hypertension increases rupture risk.
- Gently palpate for a pulsating mass in the periumbilical area and auscultate for a bruit; avoid deep palpation to prevent rupture.
- Assess peripheral circulation (pulses, color, temperature) and note any abdominal or lower back pain.
- Evaluate cardiac and respiratory function through physical examination and tests (e.g., ECG, lung function tests) due to common comorbidities.
Interventions
- Administer prescribed antihypertensive medications to maintain BP within a safe range.
- Encourage smoking cessation for at least 4 weeks before surgery to improve outcomes.
- Ensure NPO status (nothing by mouth) as instructed by the surgical team (typically light foods for ≤6 hours and clear fluids for ≤2 hours before anesthesia).
- Provide patient education and emotional support to alleviate anxiety and fear.
- Ensure necessary lab work (e.g., CBC, coagulation profile, type and crossmatch) is completed, and blood products are available.
Intraoperative Nursing Management
Intraoperative care focuses on maintaining hemodynamic stability, preventing injury, and ensuring a sterile environment.
Monitoring and Interventions
- Ensure continuous invasive cardiovascular monitoring (e.g., arterial line, central venous line).
- Administer heparin before aortic clamping and protamine to reverse its effects at the end of the procedure.
- Monitor body temperature and use warming measures to maintain normothermia.
- Use cell salvage to minimize the need for allogeneic blood transfusions.
- Maintain the mean arterial pressure (MAP) as specified by the surgical team (typically >65 mmHg).
- Ensure accurate sponge and instrument counts and meticulous hemostasis.
- Assess the color of the sigmoid colon and check pedal pulses with a Doppler before closure to confirm adequate blood flow.
Postoperative Nursing Management
Postoperative care is critical for monitoring complications and facilitating recovery. Patients are typically transferred to the ICU/HDU for close observation.
Assessment and Monitoring
- Cardiovascular:Monitor vital signs closely (BP, heart rate) and manage BP to prevent stress on graft suture lines.
- Tissue Perfusion:Perform hourly checks of lower extremity pulses (palpable or Doppler signals), color, temperature, and sensation to ensure graft patency
- Renal Function:Monitor urine output hourly (>30 mL/hr is the goal) and daily renal function tests (creatinine, BUN) as the kidneys are at risk of injury
- Respiratory Function:Encourage deep breathing exercises and early mobilization to prevent respiratory complications like pneumonia
- Gastrointestinal Function:Monitor for bowel sounds and abdominal distension. Gradually advance diet from sips of water to liquid, then solid food as tolerated.
- Incision Site:Assess the abdominal and groin incisions for signs of bleeding, swelling, or infection (e.g., redness, drainage, odor, fever)
- Pain:Conduct thorough pain assessments and administer analgesics, noting that epidural analgesia may be used.
Interventions and Education
- Administer prescribed medications (e.g., antiplatelets, statins, antihypertensives) as ordered.
- Encourage early ambulation to prevent deep vein thrombosis (DVT).
- Educate the patient on activity restrictions (e.g., no heavy lifting >5-10 lbs for 6-12 weeks) and proper wound care.
- Stress the importance of ongoing follow-up with the healthcare team and immediate reporting of any signs of complications, such as sudden severe pain in the abdomen or legs.
Educate the patient and family on medication compliance, the importance of follow-up appointments, lifestyle modifications (diet, exercise), and restrictions on heavy lifting or strenuous activities to support recovery at home.
Condition at Discharge
General condition: Patient conscious and Oriented
Vital Signs: PR – 102bpm, BP – 100/60mmhg
CVS: S1 S2(+)
RS: BAE (+)
P/A: Soft
CNS: Within normal Limits
Discharge Medication (Till Review)
| Drug | Dose | Frequency |
|---|---|---|
| Tab. Ecospirin | 75mg | OD(After food ) |
| Tab. Roseday | 20 mg | OD |
| Tab. Pan | 40mg | OD (Before food) |
| Tab. Tamin | 500mg | TDS |
| Tab. Emeset | 4mg | TDS X 5 Days Only |
| Tab. Alprax | 0.25mg | OD |
| Inj.Magnex Forte | 1.5gm | OD |
| Inj. Torgocid | 400mg | OD |
| Syp. Duphalac | 15ml | OD |
| Neb. Budecort | 1 Resp | TDS |
| Neb. Glycohale | 1 Resp | TDS |
| Nephrologist advice | ||
| Tab. Nodosis GST | 500mg | BD |
| Tab. Nefrosave | 1 Tab | OD |
Conclusion
Long-term prognosis is influenced by coexisting medical conditions and lifestyle factors. Counseling risk factor reduction, especially smoking cessation, is paramount for all patients. A team-based approach involving vascular surgery, cardiology, and other specialists is vital to optimize outcomes, whether through elective repair or in the face of an emergency.
References
- NCBI Bookshelf (Stat Pearls):The article “Aortofemoral Bypass – Stat Pearls – NCBI Bookshelf” provides comprehensive information on indications, contraindications, technique, and complications.
- Johns Hopkins Medicine:The patient education materials on “Abdominal Aortic Aneurysm Repair – Johns Hopkins Medicine” offer clear overviews of the open repair procedure.
- Cleveland Clinic:The article “Aortobifemoral Bypass Surgery: What It Is & Procedure Details” details the steps of the surgery and the recovery process.
- Journal of Vascular Surgery:For peer-reviewed technical papers, articles published in the Journal of Vascular Surgery often provide specifics on various surgical approaches and outcomes.
- Sharma A, Sharma M, Dixit S, Sharma N, Sharma O. Descending thoracic aorto-bifemoral bypass for aortoiliac occlusive disease. Indian J Vasc Endovasc Surg. 2015. 2:12-5. [Full Text].
- DeCarlo C, Boitano LT, Schwartz SI, Lancaster RT, Conrad MF, Brewster DC, et al. Society for Vascular Surgery femoral runoff score is associated with limb-based patency after aortofemoral bypass. J Vasc Surg. 2021 Jul. 74 (1):124-133.e3. [QxMD MEDLINE Link].
- Stádler P, Vitásek P, Matous P, Dvorácek L. [Hybrid robot-assisted surgery, aorto-bifemoral bypass with reconstruction of incisional hernia]. Rozhl Chir. 2008 Nov. 87 (11):590-2. [QxMD MEDLINE Link]
- Helgetveit I, Krog AH. Totally laparoscopic aortobifemoral bypass surgery in the treatment of aortoiliac occlusive disease or abdominal aortic aneurysms – a systematic review and critical appraisal of literature. Vasc Health Risk Manag. 2017. 13:187-199.