Clinical practice guidelines on peripheral IV therapy practices
Deeparani Alagarsamy1, Lydia Annie2
1Deputy Nursing Superintendent, Kauvery Hospital, Radial Road, Chennai
2Chief Nursing Officer, Kauvery Hospital, Radial Road, Chennai
Background
Peripheral intravenous catheters (PIVC) are the most used intravenous devices in hospitalized patients. They are used for therapeutic purposes such as administration of medications, fluids and/or blood products as well as blood sampling purposes.
This guideline provides recommendations regarding best practice for the use and management of invasive devices based on current evidence. Peripheral IV therapy practices privileged for the nursing fraternity and particularly decision makings done by the nurses.
1. Cannula selection
Short peripheral catheters
- Choose a short peripheral catheter as follows:
- Consider the infusate characteristics (e.g., irritant, vesicant, osmolarity) in conjunction with anticipated duration of infusion therapy (e.g., less than 6days) and availability of peripheral vascular access sites.
- Do not use peripheral catheters for continuous vesicant therapy, Parenteral Nutrition, or infusates with an osmolarity greater than 900 mOsm/L.
- Select the smallest-gauge peripheral catheter that will accommodate the prescribed therapy and patient need.
- Consider a 20- to 24-gauge catheter for most infusion therapies. Peripheral catheters larger than 20 gauge are more likely to cause phlebitis.
- Consider a 22- to 24- gauge catheter for neonates, pediatric patients, and older adults to minimize insertion-related trauma.
- Consider a larger-gauge catheter (16-20 gauge) when rapid fluid replacement is required, such as with trauma patients, or a fenestrated catheter for a contrast-based radiographic study.
- Use a 20- to 24- gauge catheter based on vein size for blood transfusion: when rapid transfusion is required, a larger-size catheter gauge is recommended
- Use steel winged devices only for single-dose administration. The device is not left in place.
| Gauge | Length | Uses | Considerations |
|---|---|---|---|
| 24 (Yellow) | 19 mm | Neonates, pediatric, elderly, hematology/oncology patients | Suitable for extremely small veins, slow flow rates |
| 22 (Blue) | 25 mm | Pediatric, elderly, hematology & oncology patients | Easy to insert, suitable for small or fragile veins, short lengths. Can use for blood products & all IV fluids & medications. |
| 20 (Pink) | 25 mm | Adolescents, adults, elderly | Mostly used for all IV fluids & medications & blood products |
| 18 (Green) | 32 mm | Adults | Suitable for the administration of viscous fluids (e.g., blood) or when high flow is required |
| 16 (Gray) | 32 mm | Adults / Maternity patients | Suitable for administration of large quantities of IV fluid, rapid flow rate, painful at insertion, requires a large vein |
- Selecting appropriate gauge and length with the fewest number of lumen and least invasive device accommodation and management of prescribed therapy.
- Large bore needles to be used for blood transfusion and in emergency fluid resuscitation e.g. Hypovolemic shock, DKA etc.
- High risk medication & inotropes are administered through EJV line / central line
- Vascular access bundle care (for prevention of complications) should be followed.
- Disinfect hands prior to all line interventions
- Use chlorhexidine to disinfect lines, connections and skin.
- Use a 2 % chlorhexidine to clean the needle free access device (e.g. smart site) use chlorhexidine (e.g. dressing change, port access)
- Allow to air dry approximately 30 seconds – do not wipe skin to dry
- Use aseptic technique when accessing lines.
- Low risk procedure should be performed using non –touch technique
- High risk procedure should be performed using full sterile technique
2. Skin preparation: Insertion site
- Hair at the insertion site should only be removed by the Nurse (prior to antiseptic application), using clippers/scissors (not shaved) to improve adherence of the dressing.
- A solution containing 2% chlorhexidine gluconate (CHG) in ≥ 70% (ethyl or isopropyl) alcohol (alcoholic chlorhexidine) should be used for preparation of the insertion site.
- If alcohol is contraindicated (e.g. allergy, sensitivity, skin condition) clinicians should use aqueous povidone-iodine 10% or sterile normal saline 0.9% (NB: The drying time for aqueous based antiseptics is longer than alcohol-based products).
3. Catheter fixation
- Poor PIVC securement has been observed to increase risk of phlebitis, infection, occlusion, infiltration and
- The catheter should be stabilized by the Nurse with a transparent dressing and sterile adhesive tape or sterile adhesive/wound closure strips, to prevent catheter dislodgement
4. Flushing policy
Flush all VADs with preservative-free 0.9% sodium chloride.
- Use a minimum volume equal to twice the internal volume of the catheter system (e.g., catheter plus add-on devices). Larger volumes may remove more fibrin deposits, drug precipitate, and other debris from the lumen. Factors to consider when choosing the flush volume include the type and size of catheter, age of the patient, and type of infusion therapy being given. Infusion of blood components, parenteral nutrition, contrast media, and other viscous solutions may require larger flush volumes.
- If bacteriostatic 0.9% sodium chloride is used, limit flush volume to no more than 30 mL in a 24-hour period to reduce the possible toxic effects of the preservative, benzyl alcohol.
- Use only preservative-free solutions for flushing all VADs in neonates to prevent toxicity.
- Use 5% dextrose in water followed by preservative- free 0.9% sodium chloride (USP) when the medication is incompatible with sodium chloride. Do not allow dextrose to reside in the catheter lumen as it provides nutrients for biofilm growth.
- Do not use sterile water for flushing VADs.
5. Labeling (ISMP– Safe practice guidelines for Adult IV push medications)
- Appropriately label all prepared syringes of IV push medications or solutions, unless the medication or solution is prepared at the patient’s bedside and is immediately administered to the patient without any break in the process.
- If the nurses need to prepare and administer more than one syringe of medication or solution to a single patient at the bedside
- Prepare each medication or solution separately, and immediately administer it before preparing the next syringe
- If preparing several IV push medications at a time for sequential IV push administration, label each syringe as it is being prepared, prior to the preparation of any subsequent syringes.
- Alternatively, if a nurse prepares one or more medications or solutions away from the patient’s bedside, immediately label each syringe, one at a time, before preparing the next medication or solution.
- Bring only one patient’s labeled syringe(s) to the bedside for administration.
- It is not safe to prepare a syringe away from the patient’s bedside and carry it unlabeled to the bedside, even if the intent is to administer it immediately. Nurses have been unexpectedly interrupted or distracted while carrying an unlabeled syringe to the bedside, thus prone to a mix-up.
- Immediately discard any unattended, unlabeled syringes containing any type of solution.
- Never pre-label empty syringes in anticipation of use.
Discussion
Unlabeled syringes should always be considered unidentifiable unless prepared at the bedside and administered immediately by the preparer. Administration of an IV push medication from an unlabeled syringe, even if the practitioner “thinks” that they know what the unlabeled syringe contains, carries high risk and has resulted in severe patient harm and even death.
6. Replacement of peripheral and midline catheters
- There is no need to replace peripheral catheters unless when clinically indicated
- Replace peripheral catheters in children only when clinically indicated.
- Replace midline catheters only when there is a specific indication.
7. Replacement of administration sets
- In patients not receiving blood, blood products or fat emulsions, replace administration sets that are continuously used, including secondary sets and add-on devices, no more frequently than at 96-hour intervals.
- Change intermittent administration set every 24 hours. When an intermittent infusion is repeatedly disconnected and reconnected for the infusion, there is increased risk of infection rate.
- Replace tubing used to administer blood, blood products, or fat emulsions(those combined with amino acids and glucose in a 3-in 1 admixture or infused separately) within 24 hours of initiating the infusion.
- Replace tubing is used to administer propofol infusions every 6 or 12 hours or when the vial is changed, , per the manufacturer recommendation.
- No recommendations can be made regarding the length of time a needle used to access implanted ports can remain in place.
| Primary continuous | Every 96 hours |
| Secondary | Every 96 hours |
| Primary intermittent | Every 24 hours |
| Secondary intermittent | Every 24 hours |
| TPN | Every 24 hours |
| Lipid emulsion | Every 24 hours |
| Blood /blood components | After each unit of administration |
| Propofol infusions | Every 6 or 12 hours |
8.Needleless Intravascular Catheter Systems
- Change the needleless components at least as frequently as the administration set. There is no benefit to changing these more frequently than every 72 hours.
- Change needleless connectors no more frequently than every 72 hours or according to manufacturer’s recommendations for the purpose of reducing infection rates.
- Ensure that all components of the system are compatible to minimize leaks and breaks in the system.
- Minimize contamination risk by scrubbing the access port with an appropriate antiseptic (chlorhexidine, povidone iodine, an iodophor, or 70% alcohol) and accessing the port only with sterile devices.
- Use a needleless system to access IV tubing.
- When needleless systems are used, a split septum valve may be preferred over some mechanical valves due to increased risk of infection with the mechanical valves.
9.VAD Removal
Peripheral IV catheters
For paediatric and adult patients when clinically indicated based on the findings from site assessment /clinical symptoms
- Pain/tenderness
- Changes in colour
- Changes in skin temperature
- Oedema
- Induration
- Leakage of fluid
- Resistance when flushing/absence of blood return
Remove the Peripheral catheter if it is no longer included in the plan of care or has been not been used for 24 hours or more.
In the event of extravasation aspirate vesicant medications prior to removal of catheter
10.Common complications are
10.1. Infiltration
Infiltration occurs when I.V. fluid or medications leak into the surrounding tissue. Infiltration can be caused by improper placement or dislodgment of the catheter. Patient movement can cause the catheter to slip out or through the blood vessel lumen.
Signs and symptoms
- Swelling, discomfort, burning, and/or tightness
- Cool skin and blanching
- Decreased or stopped flow rate
Prevention
- Select an appropriate I.V. site, avoiding areas of flexion.
- Use proper venipuncture technique.
- Follow your facility policy for securing the I.V. catheter.
- Observe the I.V. site frequently.
- Advise the patient to report any swelling or tenderness at the I.V. site.
Management
- Immediately stop the infusion and remove the device.
- Assess the distal area to the VAD site for capillary refill, sensation, and motor function.
- Elevate the limb/extremity to encourage lymphatic reabsorption of the solution/medication. Increase patient comfort; a warm compress may be applied.
- Perform venipuncture in a different location and restart the infusion, as ordered.
- Check the site frequently and use a skin marker, outline the area with visible signs of infiltration to allow for assessing changes.
- Elevate the extremity to encourage lymphatic reabsorption of the solution/medication.
- Document your findings and interventions performed.
10.2. Extravasation
Extravasation is the leaking of vesicant drugs into surrounding tissue. Extravasation can cause severe local tissue damage, possibly leading to delayed healing, infection, tissue necrosis, disfigurement, loss of function, and even amputation.
Signs and symptoms
- Blanching, burning, or discomfort at the I.V. site
- Cool skin around the I.V. site
- Swelling at or above the I.V. site
- Blistering and/or skin sloughing
Prevention
- Avoid veins that are small and/or fragile, veins in areas of flexion, veins in extremities with preexisting edema, or veins in areas with known neurologic impairment.
- Be aware of vesicant medications, such as certain antineoplastic drugs (doxorubicin, vinblastine, and vincristine), and hydroxyzine, promethazine, digoxin, and dopamine.
- Follow your facility policy regarding vesicant administration via a peripheral I.V.; some institutions require that vesicants are administered via a central venous access device only.
- Give vesicants last when multiple drugs are ordered.
- Strictly adhere to proper administration techniques.
Management
- Stop the I.V. flow and remove the I.V. line, unless the catheter remains in place to administer the antidote.
- Estimate the amount of extravasation solution and notify the prescriber.
- Administer the appropriate antidote according to Prescriber advice.
- Elevate the extremity.
- Perform frequent assessments of sensation, motor function, and circulation of the affected extremity.
- Record the extravasation site, your patient’s symptoms, the estimated amount of extravasation solution, and the treatment.
- Follow the manufacturer’s recommendations to apply either cold or warm compresses to the affected area.
- The need for consultant escalation is based on clinical signs and symptoms and their progress e.g. tissue-destroying nature
Education the patient and caregivers about:
- The risk of receiving vesicant medication prior to administration, emphasizing the specific signs and symptoms to immediately report.
- Changes that should be reported to health care professionals (changes in extreme mobility and sensation, elevated temperature and other signs of infection).
10.3.Phlebitis
Phlebitis is inflammation of a vein. It is usually associated with acidic or alkaline solutions or solutions that have a high osmolarity. Phlebitis can also occur because of vein trauma during insertion, use of an inappropriate I.V. catheter size for the vein, or prolonged use of the same I.V.site.
Signs and symptoms
- Redness or tenderness at the site of the tip of the catheter or along the path of the vein
- Puffy area over the vein
- Warmth around the insertion site
Prevention
- Use proper venipuncture technique.
- Use a trusted drug reference or consult with the pharmacist for instructions on drug dilution, when necessary.
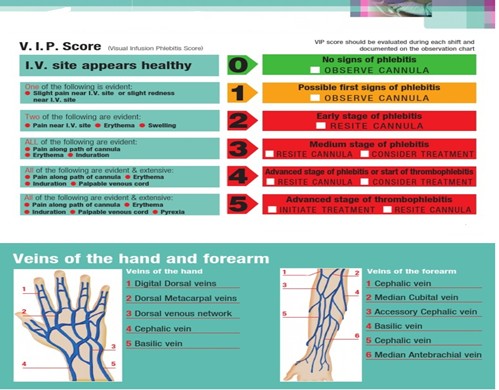
- Monitor administration rates and inspect the I.V. site frequently and use standardized tools (VIP scale) can be used for clinical evaluation.
Management
- Stop the infusion at the first sign of redness or pain.
- Apply warm compresses to the area, and elevate the limb
- If phlebitis is present, identify the possible etiology such as chemical, mechanical, infectious or post-transfusion
- Document your patient’s condition and interventions.
- If indicated, insert a new catheter at a different site, preferably on the opposite arm, using a larger vein or a smaller device and restart the infusion.
10.4. Hypersensitivity
An immediate, severe hypersensitivity reaction can be life threatening, so prompt recognition and treatment are imperative.
Signs and Symptoms
- Sudden fever
- Joint swelling
- Rash and urticaria
- Bronchospasm
- Wheezing
Prevention
- Ask the patient about personal and family history of allergies.
- For infants younger than 3 months, ask the mother about her allergy history because maternal antibodies may still be present.
- Stay with the patient for five to 10 minutes to detect early signs and symptoms of hypersensitivity.
- If the patient is receiving the drug for the first or second time, check him every five to 10 minutes or according to your facility’s policy.
Management
- Discontinue the infusion and notify the prescriber immediately.
- Administer medications as ordered.
- Monitor the patient’s vital signs and provide emotional support.
10.5. Infection
Local or systemic infection is another potential complication of I.V. therapy.
Signs and symptoms
- Redness and discharge at the I.V. site
- Elevated temperature
Prevention
- Perform hand hygiene, don gloves, and use aseptic technique during I.V. insertion.
- Clean the site with approved skin antiseptic before inserting I.V. catheter.
- Ensure careful hand hygiene before any contact with the infusion system or the patient.
- Clean injection ports before each use.
- Follow your institution’s policy for dressing changes and changing of the solution and administration set.
Management
- Stop the infusion and notify the prescriber.
- Remove the device, and culture the site and catheter as ordered.
- Administer medications as prescribed.
- Monitor the patient’s vital signs.
10.6. Air embolism
Air is always purged from syringes, administration sets, needleless connectors and any other add on devices.
Signs and symptoms
- Sudden onset of dyspnea
- Continued coughing
- Breathlessness
- Chest pain
- Hypotension
- Tachyarrhythmias
- Wheezing
- Tachypnea
- Altered mental status
- Altered speech
- Changes in facial appearance
- Numbness or paralysis
Management
- Immediately place the patient in left lateral decubitus position if not contraindicated
- Provide 100% oxygen if available
- Initiate code/MET alert
Prevention
- Priming and air purging of all administration sets
- Patient positioning and catheter occluding procedures during removal.
- To ensure VAD is clamped before changing administration sets or needleless connectors.
Other Complications are
10.7. Catheter embolism
10.8. Pulmonary embolism
10.9. Nerve injuries
11.Nurses; Responsibility
Save the Veins is the primary focus of the nurses when they plan for IV cannulation.
- Select appropriate vein and cannula size accordingly with therapeutic need
- Monitor for signs of complications
- Re-site the cannula if signs of phlebitis appear
- Educate the patients and family members to report discomfort
- Document of the site, gauge, date/time of insertion and upon removal, and reason for it must be documented
Conclusion
Peripheral IV therapy is a vital nursing procedure that provides direct access to the venous system for the administration of fluids, medications, and blood products. It is simple, cost-effective, and widely used in clinical practice. Safe and effective IV therapy requires proper vein selection, aseptic technique, careful monitoring, and timely management of complications. Nurses play a key role in ensuring patient safety, comfort, and therapeutic effectiveness through skilled insertion, maintenance, and education
12. Clinical Pathway
13. VIP score
14.Drops per minute:
Nurses need to check infusion at least every hour to ensure that the indicated mL per hour has been infused and that IV patency is maintained
Drops per minute calculated by the following formula:
Total infusion volume × Drop factor
Drops/minute = -------------------------------------------
Total time of infusion in minutes
References:
1. ISMP, Safe Practice Guidelines for Adult IV Push Medications,2015.
2. CDC – Intravascular Catheter-related Infection (BSI) Prevention Guidelines, Health Care Providers, April 12, 2024
3. Lisa Bonsall, MSN, RN, CRNP, Feb 9, 2015, Complications of Peripheral I.V. Therapy, Nursing center blog
4. Wolters Kluwer “Infusion Nurses society”, Norwood,2016.
- Standard 26, Vascular Access device(VAD) planning, S51.
- Standard 33, Vascular site preparation & Device placement, S64.
- Standard 40, Flushing & Locking, S77.
- Standard 42, Administration set change, S84.