Total Parenteral Nutrition: A comprehensive review
Uday Varma
Consultant in Anesthesia & Critical care, Kauvery Hospital, Hosur, Tamil Nadu
Background
Until the early 1960s, the use of intravenous nutrition was restricted to high concentrations of Dextrose and Electrolytes. In 1962, Wretlind and colleagues developed Lipid Infusions as the principle source of calories for parenteral feeding.
In 1966, Dudrick and Rhoads developed Parenteral Nutrition (PN) for patients who had lost their small bowel. In 1976, Solassol and Joyeux developed the three-in-one mixture by putting Sugars, Lipids and Amino Acids in a single bag.
In 1978, Shils and colleagues and Jeejeebhoy and colleagues developed ‘home’ PN to reduce costs.
Nutrition
Nutrition (also called nourishment or aliment) is the provision, to cells and organisms, of the materials necessary (in the form of food) to support life. Human nutrition is the provision to obtain the essential nutrients necessary to support life and health. Nutrients are the substances that are not synthesized in sufficient quantity in the body and therefore must be supplied from diet.
Macronutrients: Carbohydrates, Fats, Protein, Dietary fiber and Water.
Micronutrients: Vitamins, Minerals and Trace elements .
Types of Nutrition
Enteral Nutrition:
- Nutritional support via placement through the Nose, Esophagus, Stomach, or Intestines (Duodenum Or Jejunum)
- Tube feedings
- Must have functioning GI tract
- If the gut works, use it!
2. Parenteral Nutrition
Components are in elemental or “Pre-digested” form
- Protein as Amino Acids.
- Carbohydrates as Dextrose.
- Fat as Lipid Emulsion.
- Electrolytes, Vitamins and Minerals.
Parenteral Nutrition is used when the Enteral route is unable to provide or sustain sufficient caloric intake.
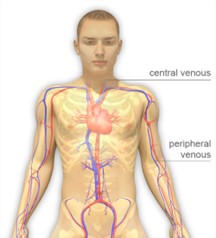
Parenteral Nutrition (Types)
Delivery of nutrients intravenously, e.g. via the bloodstream.
- Central Parenteral Nutrition: often called Total Parenteral Nutrition (TPN);
- delivered into a central vein.
- Peripheral Parenteral Nutrition (PPN): delivered into a smaller or peripheral vein.
Indications for TPN
| Short-term use | Long-term use (HOME PN) |
|---|---|
| Bowel injury, Major Trauma or Burns. | Prolonged Intestinal Failure. |
| Bowel disease (e.g. obstructions, fistulas). | Crohn’s Disease. |
| Severe Malnutrition. | Bowel Resection. |
| Nutritional preparation prior to surgery. | |
| Malabsorption - bowel cancer. | |
| Severe Pancreatitis. | |
| Malnourished patients who have high risk of Aspiration |
Contraindications
- Functional and accessible GI tract.
- Patient is taking oral diet.
- Prognosis does not warrant aggressive nutrition support (terminally ill).
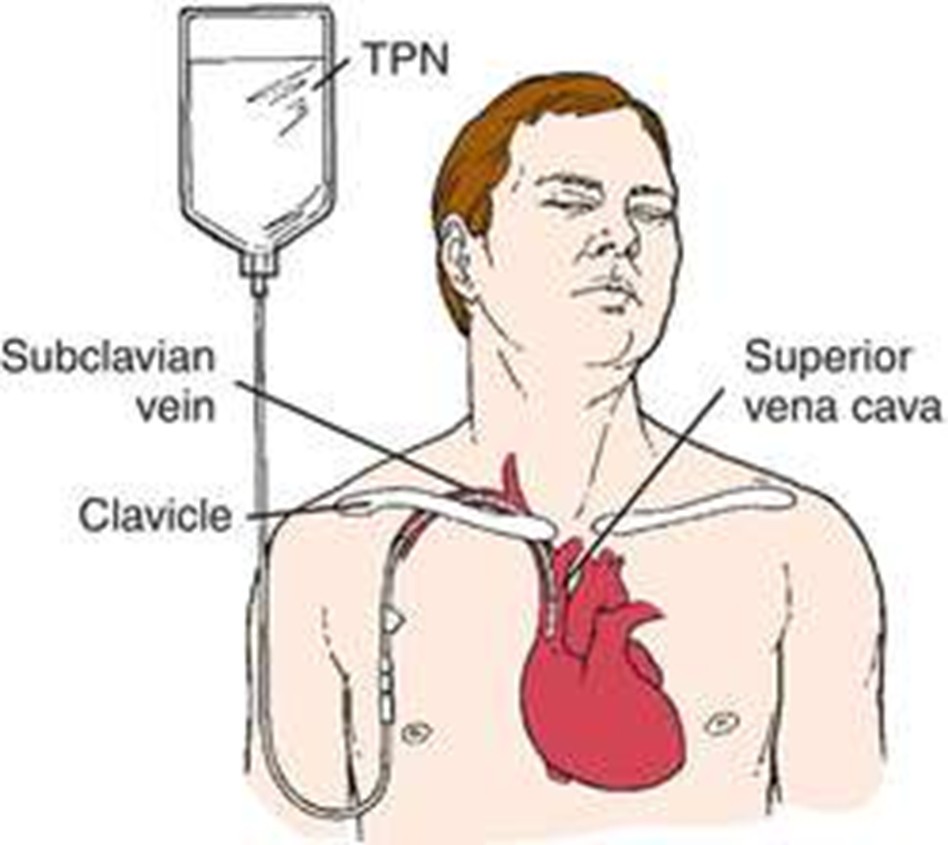
Central TPN
- Central venous catheters are the main route of TPN administration.
- The preferred entry location is the Subclavian Vein, which provides a stable site, good patient acceptability, and lower infection rates than either the internal jugular or femoral routes.
- The catheter should be a single-lumen catheter used only for TPN.
- Multiple-lumen catheters and multiple-purpose single-lumen catheters have high infection rates.
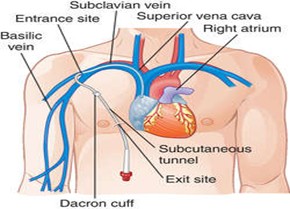
Peripherally inserted central catheters (PICCs)
- Introduced via the Basilic vein.
- Can be used both in the inpatient setting and also for longer-term outpatient therapy.
- PICC line in the outpatient setting has a lifetime of 4 to 6 weeks
Peripherally inserted central catheters (PICC’s)
| Advantages | Disadvantages |
|---|---|
| Bed side technique. | Trained personnel is needed. |
| Avoids complications of central venous catheter. | Line blockage. |
| Avoid multiple venous cannulations. | Mal position. |
| Hypertonic solutions can be given. | Phlebitis. |
| Line sepsis. | |
| Thrombosis. |
Subcutaneously tunneled central catheters (Hickman)
- The catheter of these devices can be inserted into the vein percutaneously (e.g., the Subclavian, Internal Jugular, Or Femoral) and then tunneled to the final skin exit site .
- Subcutaneous tract forms a barrier to bacterial encroachment and colonization.
- Tunneled catheters are desirable when frequent access is required.
Central catheter (Tunneled)
| Advantages | Disadvantages |
|---|---|
| Convenient exit site | Removal needs surgical dissection |
| Long lasting than non tunnels | Catheter related sepsis |
| Hypertonic solutions can be given |
Implanted Venous Access Device (Portacath)
Portacath is completely subcutaneous.
It is accessed by percutaneous insertion of a special low-profile needle (Huber needle) Which passes through the self-sealing diaphragm of the device into the chamber.
Peripheral TPN
- Peripheral veins cannot tolerate an osmolarity of more than 750 mOsm/L (the equivalent of 12.5% dextrose) .
- The fluid volume that can be tolerated limits the caloric intake.
- Therefore, this route is used mainly for supplementation or short-term feeding.
- Typically, PPN is used for short periods (<2 weeks).
Requirements
Energy
- Basal energy requirement is the function of the individual’s weight, age, gender, activity level and the disease process.
- The major components of energy output are resting energy expenditure and physical activity; minor sources include the energy cost of metabolizing food and shivering thermogenesis.
- Basal Energy Expenditure required (kcal/day) = 25 * body weight in kgs
Average energy intake is about
- 2600 kcal/d for Men and
- 1900 kcal/d for Female,
Though these estimates vary with body size and activity level.
Formula for estimating BEE (Basal Energy Expenditure) are useful for assessing the energy needs of an individual whose weight is stable:
- For Males, BEE= 900 + 10 m , and
- For Females, BEE= 700 + 7 m, where m is Mass in kilograms.
Calculated BEE is the adjusted for physical activity level
(multiplying by 1.2 for sedentary, 1.4 for moderately active and 1.8 for very active)
Caloric Requirement
Basal Energy Expenditure
| Adults (18-65) | 20-30 kcal/kg |
| Elderly (65+) | 25 kcal/kg |
| For burns Patients | 30-35kcal/kg |
Other factors
| Pregnancy Add | 300 kcal/day |
| Lactation Add | 500 kcal/day |
| Obese or Super obese | 15-20 kcal/kg |
Estimated energy requirements for hospitalized pts based on BMI
| BMI (kg/m2) | Energy requirement (kcal/kg/d) |
|---|---|
| 15 | 35-40 |
| 15-19 | 30-35 |
| 20-24 | 20-25 |
| 25-29 | 15-20 |
| 30 and >30 | <15 |
These values are recommended for critically ill pts and obese pts; add 20% of total calories in estimating energy requirement in non-critically ill pts
Carbohydrate Requirement
- Requirement of carbohydrates is 2g/kg/day.
- 1 gram = 4.5 kcal / gm.
- Constitutes 40-50 percent of total nutrition.
- Generally, because glucose is an essential tissue fuel, Glucose and
- Amino Acids are provided parenterally until the level of resting energy expenditure is reached.
- Fats are added thereafter
Fat Requirements
- Requirement of fats is 3 g/kg/day.
- 1 gram= 9kcal/gm.
- Constitutes 30-40 percent of nutrition.
- Liver can synthesize most fatty acids, but humans lack the desaturase enzyme needed to produce n-3 and n-6 fatty acid series.
- Therefore, linoleic acid should constitute at least 2% and linolenic acid at least 0.5% of daily caloric intake to prevent essential fatty acid deficiency.
Protein Requirement
- The standard Enteral and Parenteral formulas contain protein of high biological value and meet the requirements for the eight essential amino acids.
- Protein or nitrogen balance provides a measure of feeding efficacy of PN or EN.
- Calculated as – Recommended daily protein intake in grams, (Ideal Body weight in kilograms) ×4(g/day)
- Additional protein intake may be needed to compensate for excess protein loss in specific patient population such as
- Burn injuries,
- Open wounds,
- Protein losing Enteropathy/Nephropathy.
A lower protein intake may be necessary in patient with chronic renal insufficiency who are not treated by dialysis and certain patients with hepatic encephalopathy.
Nitrogen Balance
- Because protein is 16% nitrogen, each gram of urinary nitrogen (UN)represents 6.25 gram of degraded protein.
- Total body Nitrogen (N) balance can be determined as follows : N Balance (g) = ( Protein intake(g) / 6.25) – (UUN + 4 ).
(Where UUN is Urinary Urea Nitrogen excretion (in grams) in 24 hrs. Factor 4 represents daily nitrogen loss (in grams) other than UUN)
- If UUN is greater than 30 (g/24 hrs), a factor of 6 is more appropriate for the daily nitrogen losses other than UUN.
- The goal of nitrogen balance is to maintain a positive balance of 4 – 6 grms
Amino acid solutions
- Amino acid solutions are mixed together with the dextrose solutions to provide the daily protein requirements.
- A variety of amino acid solutions are available for specific clinical settings.
- The standard amino acid solutions contain approximately 50% essential amino acids and 50% nonessential + semi essential amino acids.
- The nitrogen in essential amino acids is partially recycled for the production of nonessential amino acids.
- So metabolism of essential amino acids produces less of a rise in the blood urea nitrogen concentration than metabolism of nonessential amino acids.
- amino acid solutions designed for use in renal failure are rich in essential amino acids
Glutamine
- Glutamine is the principle metabolic fuel for intestinal epithelial cells.
- Glutamine-supplemented TPN has an important role in maintaining the functional integrity of the bowel mucosa and preventing bacterial translocation.
- Glutamine is formed when glutamic acid combines with ammonia in the presence of the enzyme glutamine synthetase.
- Glutamic acid is given as exogenous source of glutamine.
Lipid Emulsions
- Intravenous lipid emulsions consist of submicron droplets (=0.45 mm) of cholesterol and phospholipids surrounding a core of long-chain triglycerides.
- The triglycerides are derived from vegetable oils (safflower or soybean oils) and are rich in linoleic acid, an essential polyunsaturated fatty acid lipid emulsions are available in 10% and 20% strengths (the percentage refers to grams of triglyceride per 100 mL of solution)
- The 10% emulsions provide approximately 1 kcal/mL, and the 20% emulsions provide 2 kcal/mL.
- Unlike the hypertonic dextrose solutions, lipid emulsions are roughly isotonic to plasma Can be infused through peripheral veins.
- The lipid emulsions are available in unit volumes of 50 to 500 mL .
- They can be infused separately (at a maximum rate of 50 mL/hour) or added to the dextrose–amino acid mixtures.
- The triglycerides introduced into the bloodstream are not cleared for 8 to 10 hours, and lipid infusions often produce a transient, lipemic-appearing (whitish) plasma.
Lipid Restriction
- Lipids are used to provide up to 30% of the daily (nonprotein) calorie requirements.
- Dietary lipids are oxidation-prone and can promote oxidant-induced cell injury.
- Use of lipids in critically ill patients (who often have high oxidation rates) should be restricted.
- Minimal amounts (4% of calorie) of lipid infusion is necessary to prevent essential fatty acid deficiency (cardiomyopathy, skeletal muscle myopathy).
Additives
Electrolytes
- Most electrolyte mixtures contain sodium, chloride, potassium, and magnesium; they also may contain calcium and phosphorous.
- The daily requirement for specific electrolyte can be specified in the TPN orders.
- If no electrolyte requirements are specified, the electrolytes are added to replace normal daily electrolyte losses.
Electrolytes Daily Requirement
| Sodium | 70 – 100 mEq/day |
| Chloride | 70 – 100 mEq/day |
| Potassium | 70 – 100 mEq/day |
| Calcium | 10 – 20 mEq/day |
| Magnesium | 15 – 20 mEq/day |
| Phosphorus | 40 - 60 mEq/day |
| Acetate | 0 – 60 mEq/day |
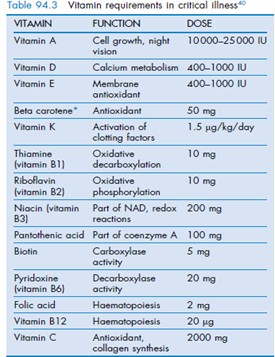
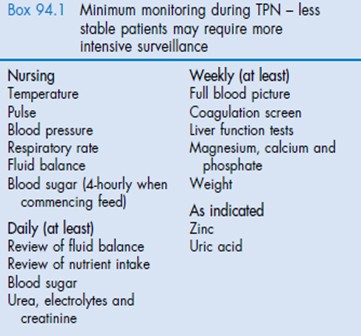
Vitamins
- Aqueous multivitamin preparations are added to the dextrose–amino acid mixtures.
- One unit vial of a standard multivitamin preparation will provide the normal daily requirements for most vitamins.
- Enhanced vitamin requirements in hypermetabolic patients in the ICU may not be satisfied.
- Some vitamins are degraded before they are delivered.
- Some examples are riboflavin and pyridoxine (which are degraded by light) and thiamine (which is degraded by sulfites used as preservatives for amino acid solutions)
Trace Elements
- A variety of trace element additives are available
- Most trace element mixtures contain chromium, copper, manganese, and zinc, but they do not contain iron and iodine.
- Some mixtures contain selenium, which has a role in protection against oxidation injury.
- Routine administration of iron is not recommended in critically ill patients because of the pro-oxidant actions of iron
Creating a TPN Regimen
Step 1
- The first step is to estimate the daily protein and calorie requirements.
- Daily Calorie Requirement will be 25 kcal/kg, and the Daily Protein Requirement will be 1.4 g/kg.
Therefore, for the 70-kg Patient, the Protein and Calorie requirements are as follows:
- Calorie requirement = 25 (kcal/day) × 70 (kg) = 1750kcal/day
- Protein requirement = 1.4(g/day) ×70 (kg) = 98g/day
Step 2
- The next step is to take a standard mixture of 10% amino acids (500 mL) and 50% dextrose (500 mL) and determine the volume of this mixture that is needed to deliver the estimated daily protein requirement.
- Dextrose–amino acid mixture is referred to as A10 – D50,
which actually contains
- 5% amino acids (50 grams of protein per liter) and
- 25% dextrose (250 grams’ dextrose per liter).
Therefore, the volume of the A10 – D50 mixture needed to provide the daily protein requirement is
Volume of A10–D50 = 98g/day = 1.9L/day 50g/L
If this mixture is infused continuously over 24 hours, the infusion rate will be 1900 mL/24 hours = 81 mL/hour.
Step 3
- Using the total daily volume of the dextrose–amino acid mixture determined in Step 2, the total calories that will be provided by the dextrose in the mixture is calculated.
- Amount of Dextrose = 250 (g/L) X 1.9 (L/day) = 475g/day
- Dextrose Calories = 475(g/day) X 3.4 (kcal/g) = 1615kcal/day
- The remaining 135 k calories can be provided by – intravenous lipid emulsion.
Step 4
- If a 10% lipid emulsion (1 kcal/mL) is used to provide 135 kcal/day, the daily volume of the lipid emulsion will be 135 mL/day.
- The volume can be infused at half the maximum recommended rate
(50 mL/hour) to minimize the tendency to develop lipemic serum during the infusion & adjusted to 150 ml/day to avoid wastage as lipid emulsion is available in unit volumes of 50 ml.
Step 5
The daily TPN orders for the previous example can then be written as follows:
- Provide standard TPN with A10–D50 to run at 80 mL/hour.
- Add standard electrolytes, multivitamins, and trace elements.
- Give 10% Intralipid: 150 mL to infuse over 6 hours
Total Nutrient Admixture
- The example just presented applies to the separate administration of dextrose–amino acid mixtures and lipid emulsions.
- Another practice that is gaining popularity is to add the nutrient solutions and additives together to form a total nutrient admixture (TNA).
Advantages of TNA
- Limits the number of central venous catheter violations and chance for contamination
- Produces a hyperosmolar environment in the TNA solution that protects against bacterial growth.
- Allows continuous infusion, thereby ensuring lipid administration at a safe rate (<0.11 g/kg/hr).
Complications of TPN
Complications of central venous catheterization
- Pneumothorax
- Hemothorax,
- Brachial Plexus injury
- Catheter Misplacement in the Azygos Vein, Right Ventricle, or Retrograde into the Jugular Vein.
- Peripheral venous access whether via a short peripheral venous catheter can result in Thrombophlebitis
1). Catheter-related infections
- These are the major venous access complication encountered with TPN.
- Infections are uncommon during the first 72 hours after insertion but then increase in incidence.
- Most often caused by Staphylococcus epidermidis or Staphylococcus aureus or Candida
- The incidence of central venous catheter–related bloodstream infections ranges from 0.3 to 30 per 1000 catheter-days .
- Mortality attributed to catheter-related infections is as high as 25%
- To prevent infective complications,
- Any manipulation of the catheter or line must be performed using sterile procedures.
- The site must be examined regularly for signs of erythema and infection.
2). Metabolic Complications
- Hyperglycemia is a common problem, especially with severe stress, steroid use, and diabetes mellitus requiring treatment with insulin.
- It is preferable to administer insulin than to reduce the glucose intake unless there is excessive hyperglycemia (>250 mg/dL) despite high insulin doses.
- Insulin treatment can reduce serum potassium and phosphate concentrations, which require repletion.
- As the stress response abates, the degree of glucose intolerance lessens and insulin requirements drop.
- The blood glucose should be closely monitored to prevent hypoglycemia
- Hypoglycemia can occur on the abrupt discontinuation of continuous feedings containing significant amounts of carbohydrate.
- Continuous feedings result in high blood insulin concentrations so that hypoglycemia intervenes when the carbohydrate intake stops.
- Therefore, when stopping continuous parenteral and enteral nutrition, any concomitant insulin infusion must be stopped, intravenous glucose should be infused, and blood glucose monitored frequently.
- The practice of using TPN solutions containing lower glucose:lipid ratios (70:30 to 50:50) has reduced the incidence of hypoglycemia after abrupt discontinuation .
Refeeding Syndrome
- Hypophosphatemia occurs when tissues begin to rebuild and is especially problematic if inadequate phosphate intake is provided in malnourished patients when TPN or enteral feeds are started.
- Hypophosphatemia may lead to major muscle (including respiratory muscle) weakness and glucose intolerance because phosphate is a vital component of tissue membranes, enzymes, and nucleosides, especially ATP.
- Concurrent hypomagnesemia, hypocalcemia, and hypokalemia may exacerbate the muscle weakness.
- Chronic alcoholics are especially prone to hypophosphatemia.
3). Hepatic dysfunction
- Hepatic dysfunction is commonly observed in patients receiving TPN.
- These disorders occupy a spectrum ranging from simple elevations in liver function test results to cirrhosis.
- Most often, if hyperbilirubinemia occurs acutely in a patient receiving TPN, the cause is generally sepsis.
- Factors responsible for liver disease attributable primarily to TPN administration, remain unclear.
- Hepatic steatosis, cholestasis (presumably from lack of enteral stimulation and reduced release of cholecystokinin), and the presence of chronic inflammation have all been implicated as relevant mechanisms.
- TPN-specific factors include excessive glucose or insulin administration (with increased hepatic lipogenesis), excessive lipid administration (sequestration in hepatocytes), and alterations in fatty acid metabolism leading to the release of arachidonate-derived inflammatory leukotrienes.
- Deficiencies in particular nutrients, such as carnitine, choline, taurine, cysteine, and S-adenosyl methionine, have also been implicated in TPN-related liver disease .
- Addition of 1 to 2 g of carnitine to standard TPN, especially during long-term administration is recommended to prevent liver dysfunction.
- The use of oral ursodeoxycholic acid (e.g., 500 mg at bedtime or twice daily) is useful to resolve cholestasis when liver function test abnormalities are observed during chronic TPN administration
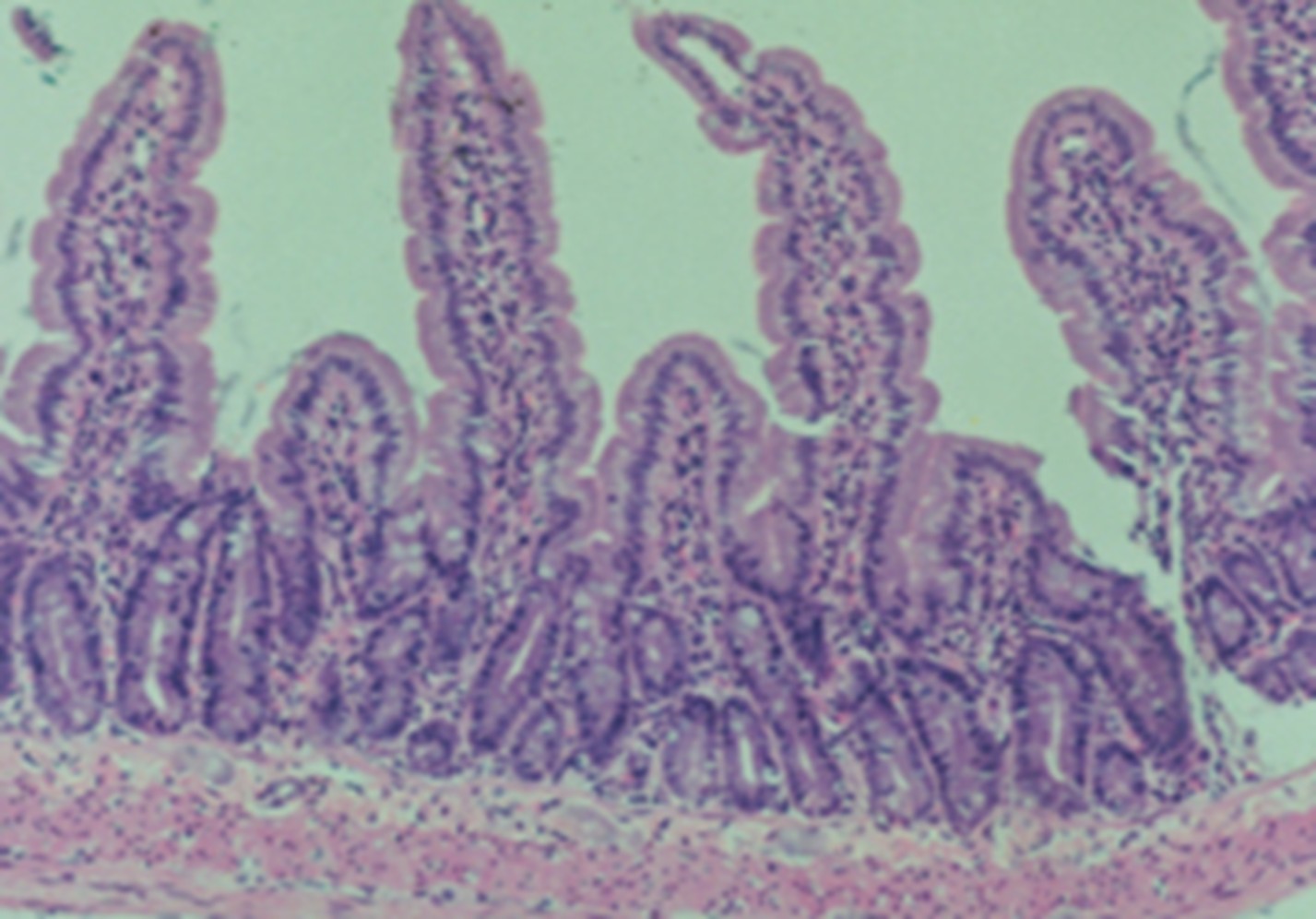
4). Mucosal Atrophy
- The absence of bulk nutrients in the bowel produces atrophy and disruption of the bowel mucosa.
- These changes can predispose to translocation of enteric pathogens across the bowel mucosa and subsequent septicemia.
- Because TPN is usually accompanied by bowel rest, one of the indirect complications of TPN is bacterial translocation and sepsis of bowel origin.
- Glutamine-supplemented TPN may help reduce the risk of this complication.
5). Metabolic Bone Disease
- Patients administered TPN over prolonged periods have decreased bone mineral density (BMD).
- Patients at greatest risk are postmenopausal women, patients with long-standing malnutrition or malabsorption (e.g., Crohn’s disease), those with preexisting liver disease, or patients receiving steroids.
- TPN-associated deficiency states, such as calcium, magnesium, copper, boron or silicon, have been suggested to play a role.
- Use of bisphosphonates which prevents osteoclast-mediated bone resorption is being tried.
Enteral Nutrition
- Enteral nutrition = Administration of nutrients via the existing GIT
- EN is confined to tube feeding exclusively without regards to oral nutritional supplement
| Indications | Contraindications |
|---|---|
| 5-7 days of inadequate intake. | Intestinal Obstruction. |
| Prolonged anorexia. | Intestinal Ischaemia/Perforation. |
| Inability to take oral feedings. | Inability to access the gut. |
| Impaired intestinal function. | Severe acute pancreatitis |
| Critical illnesses. | High output proximal fistula |
| Shock |
Advantages
- Preserves gut integrity
- Possibly decreases bacterial translocation
- Preserves immunological function of gut
- Better tolerated by patient
- Less costly than TPN
Administration Sites
- Gastric
- Postpyloric
Gastric Feed
Advantages
- More Physiological
- Ease of placement
Disadvantages
- Delayed gastric emptying
- Gastroesophageal reflux and aspiration
Post-pyloric Feed
Advantages
Minimize aspiration risk.
Disadvantages
- Difficulty with placement.
- Feeding intolerance.
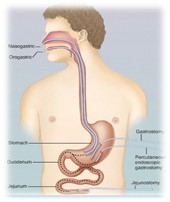
Types of feeding tubes
- Nasogastric
- Nasojejunal
- Percutaneous endoscopic gastrostomy
- Open gastrostomy
- Transgastric jejunostomy
- Jejunostomy
If tube feeding is needed for ≤ 4 to 6 wk, nasogastric or nasoenteric is usually used.
Tube feeding for > 4 to 6 wk usually requires a gastrostomy or jejunostomy tube.
Nasogastric tubes
Advantages
- Cheap
- Easy to insert
- Residual volume can be assesed.
Disadvantages
- Uncomfortable
- Easily dislodged
- Increase aspiration risk
Advantages
- Cheap
- Easy to insert
- Residual volume can be assesed.
Disadvantages
- Uncomfortable
- Easily dislodged
- Increase aspiration risk
Nasojeunal Tubes
Advantages
- Decreased risk of aspiration
- Decreased stimulus to pancreatic secretion
- Indicated – Gastric reflux, delayed gastric emptying
Disadvantages
- Not easy to place.
- Damage to gastric mucosa.
- Impaired absorption.
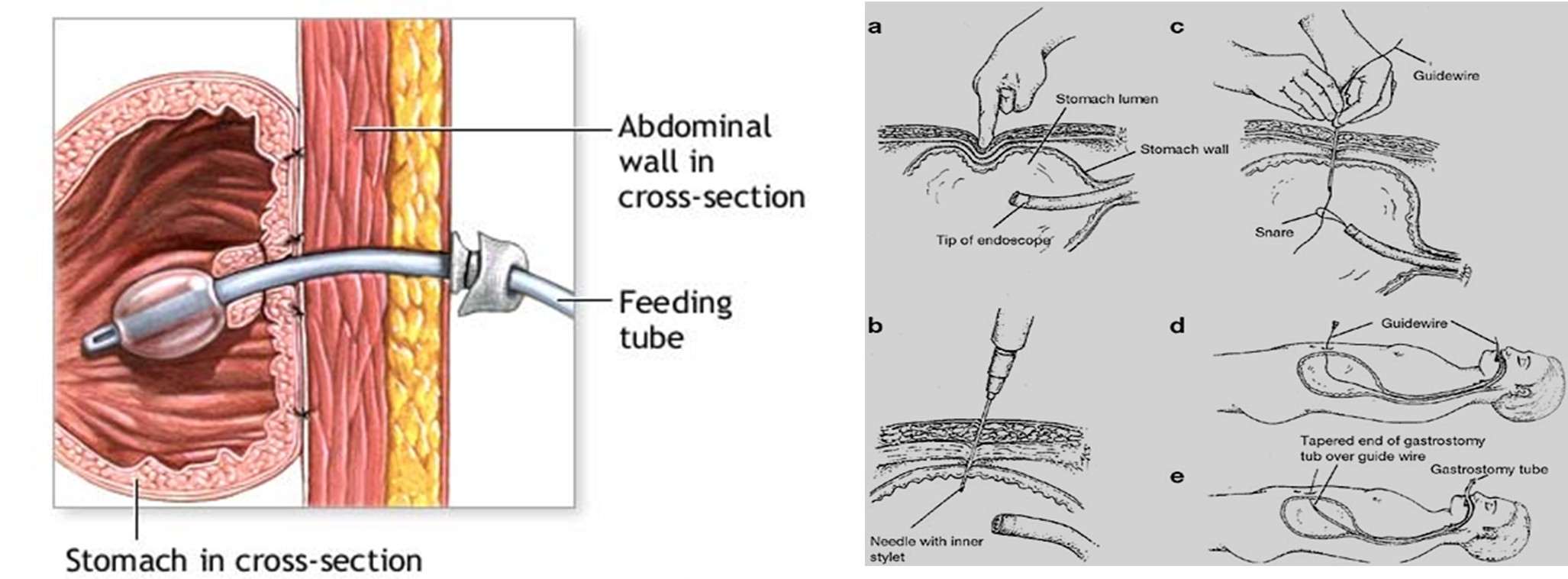
Gastrostomy
Placement of tube through abdominal wall directly into stomach.
Now a days performed by percutaneous insertion under endoscopic control known as PEG (Percutaneous Endoscopic Gastrostomy).
Contraindications
- Gastric ulcer.
- Gastric carcinoma.
- Ascites
- Coagulation disorders.
Complications
- Sepsis around PEG site.
- Nectrotizing fascitis and intraabdominal wall abscess.
- Persistent gastric fistula.
Jejunostomy
Percutaneous Endoscopic jejunostomy
- Technically difficult
- Allows concomittent jejunal feeding and gastric decompression.
Administration
Bolus Feeding
Large amount (300-400ml) is given in short time period several times daily.
Continuous Feeding
Administration into the GIT via pump or gravity, usually over 8 to 24 hours per day.
Intermittent Feeding
300 to 400 ml, 20 to 30 minutes, several times/day via gravity drip or syringe.
Feeding Protocol
Rate of administration
Gastric feeding
- Standard formula: 50 ml/hr
- Advanced by 25ml/hr every 4-8 hours until goal rate is made
- Elemental formula :25ml/hr for first 12 hour
- Advanced by 25ml/hr every 6-12 hour
Jejunal or duodenal feedings
- Standard or elemental feeding at full strength at 25 ml/hr for first 12 hours then advanced by 25ml/hr every 6-12 hours.
- Bolus feeding method not used.
Monitoring Tolerance
Gastric Feeds
- Check residual volumes every 4 hours.
- Hold tube feeding residual greater than 200ml.
- Reinfuse residual recheck in 2 hours .
- Feeds should be held if increasing abdominal distention.
Jejunal Feeds
- Monitor abdomen for distension
- bowel sounds every 4 hours
- Residual volumes are not helpful
- Hold feeds if emesis abdominal pain or distension
Complications
Tube Related
- Malposition
- Displacemant
- Blockage
- Breakage/leakage
- Local complication (erosion of skin / mucosa)
- Metabolic
- Refeeding syndrome
- Electrolyte disorder
- Vitamin mineral trace element deficiencies
Gastrointestinal
- Diarrhoea.
- Nausea & vomiting.
- Abdominal cramps.
- Aspiration.
- Constipation.
Reference
- Leah Gramlich, M.D.,1 and Peggi Guenter, Ph.D., R.N. Enteral Nutrition in Hospitalized Adults. N Engl J Med 2025; 392:1518-30. DOI: 10.1056/NEJMra2406954